ICD-10 Diagnosis Codes:
H00.021–Internal hordeolum, Right upper eyelid
H00.022–Internal hordeolum, Right lower eyelid
H00.024–Internal hordeolum, Left upper eyelid
H00.025–Internal hordeolum, Left lower eyelid
Title
Meibomian Gland Disease
Category
Inflammation Of Eyelids
Description
An abnormality of the meibomian glands commonly characterized by duct obstruction and/or changes in duct secretions.
Meibomian gland disease is also called posterior blepharitis. It refers to those manifestations primarily affecting the meibomian glands and the meibum they secrete. The condition is characterized by the following abnormal signs and symptoms:
- Puffy eyelids
- Ocular redness
- Crusty debris in the eyelashes
- Inflammed, erythematous eyelid margins
- Eyelid involvement is usually bilateral and symmetric
- Associated evaporative dry eye syndrome in 50-75% of patients
- Abnormal signs and symptoms that are usually worse in the morning
- Severe cases can produce corneal scarring, corneal neovascularization and marginal keratitis
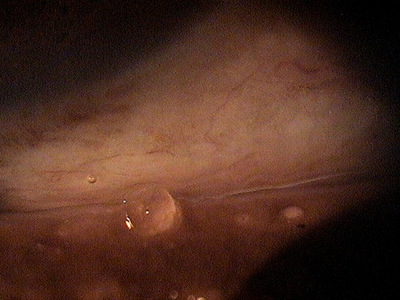
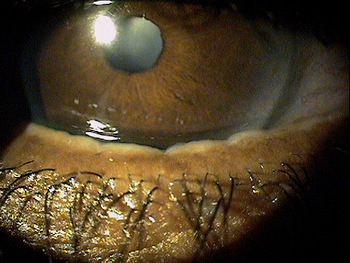
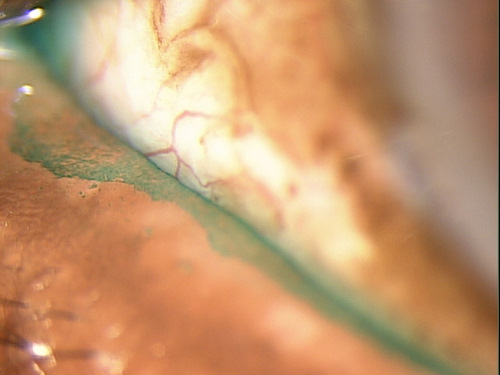
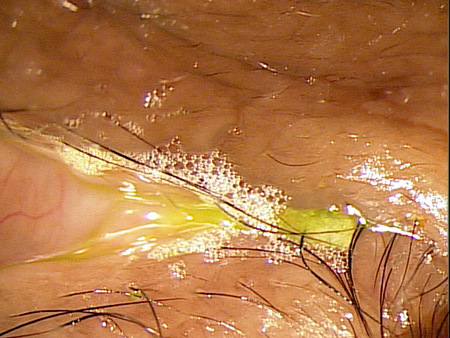
Structural Damage to the Eyelid and Eye
|
 |
|
|
|
Functional Damage to the Eye
- Fluctuating vision from the effects of an unstable tear film
- Blurred vision from corneal epitheliopathy
The main goal of the diagnostic evaluation in a patient with meibomian gland disease is to accomplish the following:
1. Stage the disease based on it’s clinical features
- Patient symptoms
- Eyelid appearance and meibomian gland secretions
- Ocular surface staining
2. Relieve ocular pain and discomfort
- Prescribe a treatment program to treat the posterior blepharitis
- Prescribe a treatment program to treat any associated dry eye syndrome
Patient History
Patients may present with any or all of the following clinical signs and symptoms:
- None
- Mild ocular discomfort
- Itching
- Photophobia
- Ocular redness
- Puffy eyelids
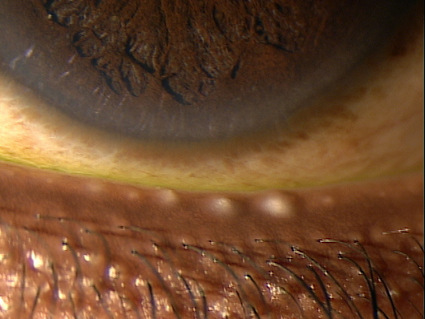
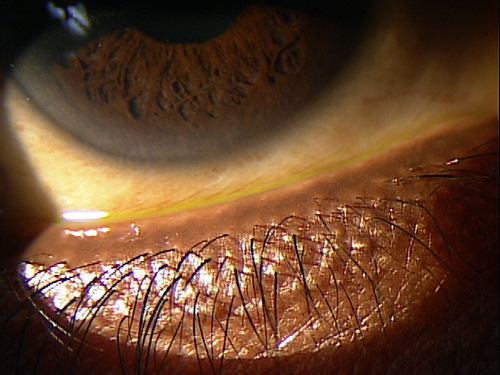
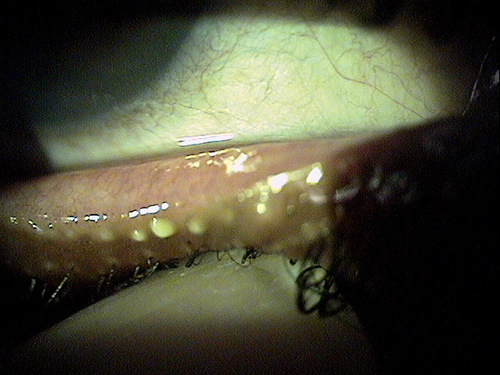
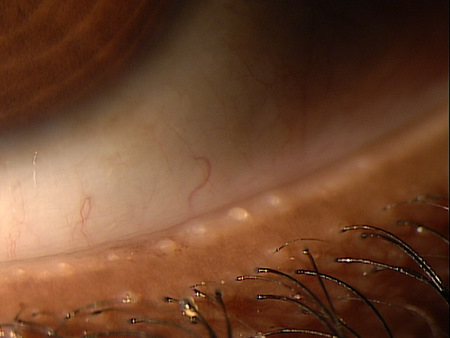
External Ocular Examination with Biomicroscopy
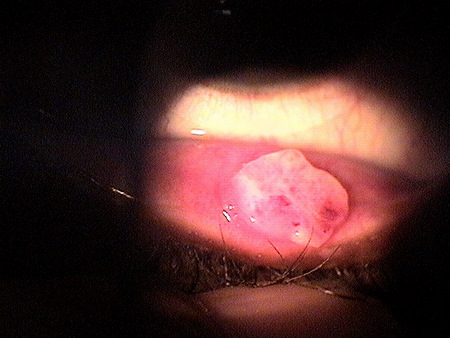
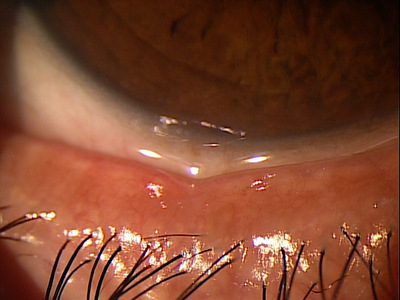
- Meibomian gland orifice plugging
- Meibomian gland duct obstruction
- Meibomian gland atrophy and dropout
- Qualitive changes in the expressed secretions
- Eyelid margin hyperemia
- Eyelid vessel telangiectasia
- Tear film frothing
DIAGNOSTIC TESTS
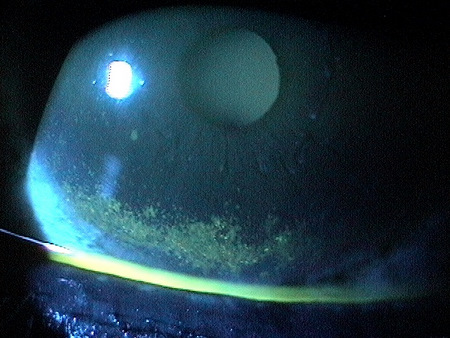
External Ocular Photography
- Document clinical appearance of the eyelid margin
- Document clinical appearance of the inferior cornea
- Help to plan treatment of meibomian gland disease
Meibomian gland disease can be categorized into four subtypes:
Primary meibomian gland disease
- Meibomian gland dropout
- Altered meibomian gland secretion
- Changes in eyelid morphology
Meibomian gland disease associated with ocular surface damage
- Staining of the cornea
- Staining of the conjunctiva
Meibomian gland disease-related evaporative dry eye
- Reduced tear-film stability
- Abnormal tear film spreading pattern
- Increased loss of water from the tear film secondary to evaporation
Meibomian gland disease associated with other ocular disorders
- Contact lens wear
- Seborrhea sicca
- Acne rosacea
- Seborrheic dermatitis
- Atropy
CHRONIC PRESENTATIONS
Best practices treatment guidelines from The International Workshop on Meibomian Gland Dysfunction suggest the following treatment options:
- Improve patient symptoms
- Reduce chronic gland inflammation
- Improve the quality of the meibum secretion
- Prevent damage to the ocular surface
- Prevent meibomian gland dropout
Palliative Treatment
- Artificial tears (non-preserved is preferred for frequent use)
- Topical emollient lubricant
- Liposomal spray
- Warm compress therapy
Topical cyclosporine (e.g., Restasis ophthalmic emulsion)
- If concurrent corneal epitheliopathy is present
- If concurrent aqueous deficiency dry eye syndrome is present
Oral tetracyclines
- Tetracycline 250 mg (4x per day for 30 days)
- Doxycycline 50-100 mg (2x per day for 30 days)
- Minocycline 50-100 mg (2x per day for 30 days)
Nutritional Treatment
- Omega-3 fatty acid dietary supplementation to decrease inflammation in the eyelids
In 2003, research presented at the 2003 Annual meeting of the Association for Research in Vision and Ophthalmology found that high dietary intake of omega-3 essential fatty acids decrease the risk of dry eye syndrome. The anti-inflammatory effects of omega-3’s also help the reduce inflammation in the eyelids.
Mechanical Treatment
- Meibomian gland therapeutic expression
Surgical Treatment
- Ductal probing of the meibomian gland
1. Pitts J. Lievens C. Put The Squeeze on Meibomian Gland Disease. 16 Sept 2009. RevOptom. http://www.revoptom.com/content/c/15811/. Last accessed August 17, 2014.
2. Stephenson M. Blepharitis: The Cause Guides to Treatment. Review of Ophthalmology. 5 Sept 2013. http://www.revophth.com/content/c/42801/. Last accessed August 17, 2014.
3. Stuart A. Managing Blepharitis: Tried-and-True and New Approaches. American Academy of Ophthalmology. http://www.aao.org/publications/eyenet/201207/cornea.cfm. Last accessed August 17, 2014.
4. Lowery S. Adult Blepharitis. Medscape/EMedicine. 20 Feb 2014. http://emedicine.medscape.com/article/1211763-overview. Last accessed August 17, 2014.
5. Kabat A. Shechtman D. Current Therapeutic Approaches to Blepharitis Management. RevOptom. 3 Mar 2011. http://www.revoptom.com/content/c/27049/. Last accessed August 17, 2014.
373.12
Hordeolum internum
92285
External ocular photography




 Print | Share
Print | Share