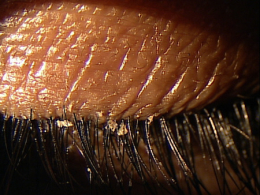
Flaking of the eyelashes in anterior blepharits
ICD-10 Diagnosis Codes:
H01.001–Blepharitis, right upper eyelid
H01.002–Blepharitis, right lower eyelid
H01.004–Blepharitis, left upper eyelid
H01.005–Blepharitis, left lower eyelid
Title
Blepharitis
Category
Inflammation Of Eyelids
Description
Blepharitis is an infection or inflammation of the anterior portion of the eyelid.
Anterior blepharitis affects the anterior portion of the eyelid margin and the eyelashes. It refers to those manifestations primarily affecting the lashes and their associated pilosebaceous glands. Bacterial and seborrheic are the most common types of anterior blepharitis, while Demodex (mites) and acne rosacea are less common causes.
The condition is characterized by the following abnormal clinical signs:
- Inflamed, erythematous eyelid margins
- Dry, crusty debris in the eyelashes
- Eyelid involvement is usually bilateral and symmetrical
- Associated evaporartive dry eye syndrome in 50-75% of patients
- If untreated, eventual lash loss (madarosis) and eyelid scarring
- Severe cases can produce corneal scarring and corneal neovascularization
Structural Damage to the Eye
For staphylococcal and seborrheic anterior blepharitis, the conditions affect the area surrounding the base of the eyelashes.
Bacteria-associated anterior blepharitis results from bacterial overgrowth, most commonly from staphylococcus epidermis and staphylococcus aureus.
- Toxic bacterial products released into the tear film stimulate the production and release of pro-inflammatory cytokines
- Subsequent chemotaxsis recruits additional inflammatory cells, triggering host-induced and organism-induced inflammation
- Bacterial-associated anterior blepharitis is recognized by its inflamed, erythematous eyelid margins and dry, crusty debris in the eyelashes, especially collarettes
Seborrheic anterior blepharitis results from a dysfunction of the pilosebaceous glands and may be related to malassezia furfur, a pathologic yeast fungus on or near the eyelash follicles.
- In seborrheic anterior blepharitis, the glands produce excessive sebum, resulting in large, greasy scales that accumulate along the hair shaft and surrounding skin
- Common sites for abnormal clinical signs include the eyebrows, glabella and anterior scalp
- Eyelid erythema is typically mild, except in severe cases
- Demodex anterior blepharitis is caused by microscopic mites (demodex folliculorum) and their waste materials clogging eyelash follicles
- Anterior blepharitis caused by acne rosacea is characterized by telangiectaic areas on the cheeks, nose, chin, and eyelid margins
Functional Damage to the Eye
- Fluctuating vision from the effects of an unstable tear film
- Blurred vision from corneal epitheliopathy
The main goal of the diagnostic evaluation in a patient with anterior blepharitis is to accomplish the following:
1. Stage the disease based on it’s clinical features
- Patient symptoms
- Eyelid appearance
- Ocular surface staining
2. Relieve ocular pain and discomfort
- Prescribe a treatment program to treat the anterior blepharitis
- Prescribe a treatment program to treat any associated dry eye syndrome
Patient History
Patients may present with any or all of the following clinical signs and symptoms:
- None
- Mild ocular discomfort
- Itching
- Photophobia
- Ocular redness
- Puffy eyelids
External Ocular Examination with Biomicroscopy
- Hard scales and crusting around the base of the eyelashes
- Mild papillary conjunctivitis
- Chronic conjunctival hyperemia
- Scarring and notching of the eyelid margin
- Madarosis, trichiasis, and poliosis
- Stye formation
- Marginal keratitis
- Phlyctenulosis
- Tear film instability
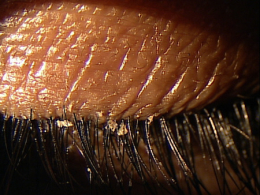 |
Clinical Appearance of the Eyelashes
|
|
 |
Clinical Appearance of the Eyelashes
|
|
 |
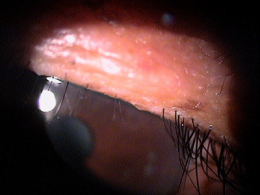
Clinical Appearance of the Palpebral Conjunctiva
|
|
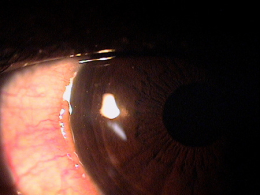 |
Clinical Appearance of the Bulbar Conjunctiva
|
|
 |
Clinical Appearance of the Eyelid Margin
|
DIAGNOSTIC TESTS
External Ocular Photography
- Document clinical appearance of the eyelid margin
- Document clinical appearance of the inferior cornea
- Help to plan treatment of meibomian gland disease
Anterior blepharitis can be categorized into four subtypes:
Stapylococcal blepharitis
- Collarettes around the base of the eyelashes
- Mild papillary conjunctivitis
- Scarring and notching of the lid margin
- Loss of eyelashes
Seborrheic blepharitis
- Hyperemia of the anterior lid margin
- Greasy anterior lid margin
- Sticking together of lashes
- Soft scales on the eyelashes and eyelid margin
Demodex-induced anterior blepharitis
- Waste material from the mites is visible at the base of the eyelashes
Acne rosacea-induced anterior blepharitis
- Characterized by telangiectasias
There are no differential diagnoses for anterior blepharitis.
The goals of treating anterior blepharitis include the following:
- Improve patient symptoms
- Reduce chronic eyelid inflammation
- Prevent damage to the ocular surface
Mechanical Treatment
- Eyelid hygiene with lid scrubs
Palliative Treatment
- Artificial tears (non-preserved is preferred for frequent use)
- Topical emollient lubricant
- Liposomal spray
- Warm compress therapy
Pharmacologic Treatment
- Topical antibiotic gel eye drops (e.g., Azasite ophthalmic solution)
- Topical cyclosporine eye drops (e.g., Restasis ophthalmic emulsion)
- Topical antibiotic/steroid eye drops (e.g., Tobradex ST or Zylet ophthalmic suspension)
- Topical steroids eye drops (e.g., Lotemax gel, FML 0.1%, or Pred forte ophthalmic suspension)
- Topical steroid/antibiotic ointment (e.g., Tobradex ophthalmic ointment)
- Topical steroid ointment (e.g., Lotemax ophthalmic ointment)
1. Stephenson M. Blepharitis: The Cause Guides to Treatment. Review of Ophthalmology. 5 Sept 2013. http://www.revophth.com/content/c/42801/. Last accessed August 17, 2014.
2. Stuart A. Managing Blepharitis: Tried-and-True and New Approaches. American Academy of Ophthalmology. http://www.aao.org/publications/eyenet/201207/cornea.cfm. Last accessed August 17, 2014.
3. Lowery S. Adult Blepharitis. Medscape/EMedicine. 20 Feb 2014. http://emedicine.medscape.com/article/1211763-overview. Last accessed August 17, 2014.
4. Kabat A. Shechtman D. Current Therapeutic Approaches to Blepharitis Management. RevOptom. 3 Mar 2011. http://www.revoptom.com/content/c/27049/. Last accessed August 17, 2014.
373.00
Blepharitis, unspecified
92285
External ocular photography




 Print | Share
Print | Share