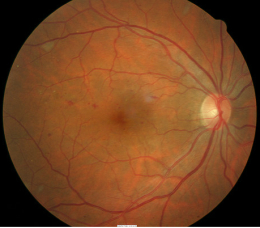
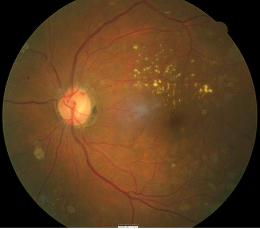
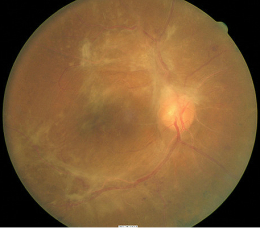
Background diabetic retinopathy imaged with fundus autofluorescence after laser surgery
ICD-10 Diagnosis Codes:
E11.319–Mild nonproliferative diabetic retinopathy, without macular edema
E11.339–Moderate nonproliferative diabetic retinopathy, without macular edema
E11.349–Severe nonproliferative diabetic retinopathy, without macular edema
Title
Diabetic Retinopathy
Category
Other Retinal Disorders
Description
Diabetic retinopathy is a disease manifestation of diabetes. The condition is defined as retinal changes associated with long-term diabetes.
Diabetes
Diabetes mellitus is a complex, multifactorial and heterogeneous group of disorders characterized by endogenous insulin deficiency and/or insulin resistance. The disease manifests itself as a state of chronic hyperglycemia with attendant microvascular and macrovascular complications.
Diabetic Retinopathy
This is the most common and most serious ophthalmic manifestation of diabetes mellitus. It is a microangiopathy affecting the retinal blood vessels, and has features of both microvascular occlusion and leakage.
- Microvascular complication of diabetes that is based on the observation of vascular changes or the presence of abnormal vascular lesions:
- Retinal vasculopathy is a response to hyperglycemia
- Microaneurysms and other vascular leakage (i.e. hard exudates and macular edema)
- Capillary occlusion, neovascularization
-
Oxidative stress is a main causative factor in diabetic microangiopathy
-
Release of inflammatory proteins, leukostasis, and programmed destruction of endothelial cells and retinal ganglion cells and axons
-
Biochemical alteration results in a breakdown in the blood-retinal barrier
Structural Damage to the Eye
- Walls of the blood vessels in the retina become fragile and weakened
- Weakened blood vessels have an increase in vascular permeability
- Lipid deposits form in the retinal tissue secondary to chronic edema
- Fluid accumulates in the macula
- Diabetic macular edema develops
Functional Damage to the Eye
- Distorted or blurred vision
- Report seeing spots or floaters in field of view
- Report dark or empty spot in the central vision
- Difficulty seeing at night
The main goal of the diagnostic evaluation in a patient with diabetic retinopathy is to accomplish the following:
- Determine the presence or absence of diabetic retinopathy
- Classify the diabetic retinopathy
- Identify and exclude differential diagnosis
- Determine if the retinopathy is clinically significant and/or vision threatening
- Prescribe a treatment program
Patient History
The severity of the symptoms or signs is varied and depends on the level of control the patient has over their diabetes. Patients can present with the following abnormal symptoms:
- Blurred vision (sudden or gradual)
- Distorted vision (sudden or gradual)
- Difficulty driving at night
- Floaters or dark spots in their field of view
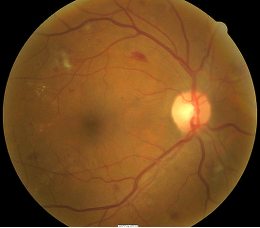
Clinical Appearance of the Retina
The retinal changes associated with diabetic retinopathy include the following:
- Hemorrhages
- Microaneurysms
- Lipid deposits
- Cotton wool spots
- Edema
- Ischemia
- Venous beading
- Intraretinal microvascular abnormalities
- Retinal thickening
- Neovascularization
- Proliferative non-inflammatory degeneration
 |
 |
DIAGNOSTIC TESTS
Fundus Photography
- To document the progress or lack of progress of diabetic retinopathy
- To document the delivery of medical treatment
- To document the response to treatment
- To help plan a treatment program
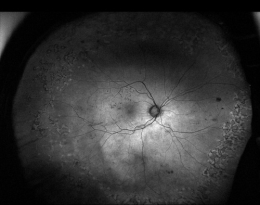
- Fundus autofluorescence imaging can be used to detect structural abnormalities and predict functional deficits before the defects appear on standard color fundus photography
- Multi-spectral imaging with the Annidis RHA System can be used to detect structural abnormalities and predict functional deficits before the defects appear on standard color fundus photography
 |
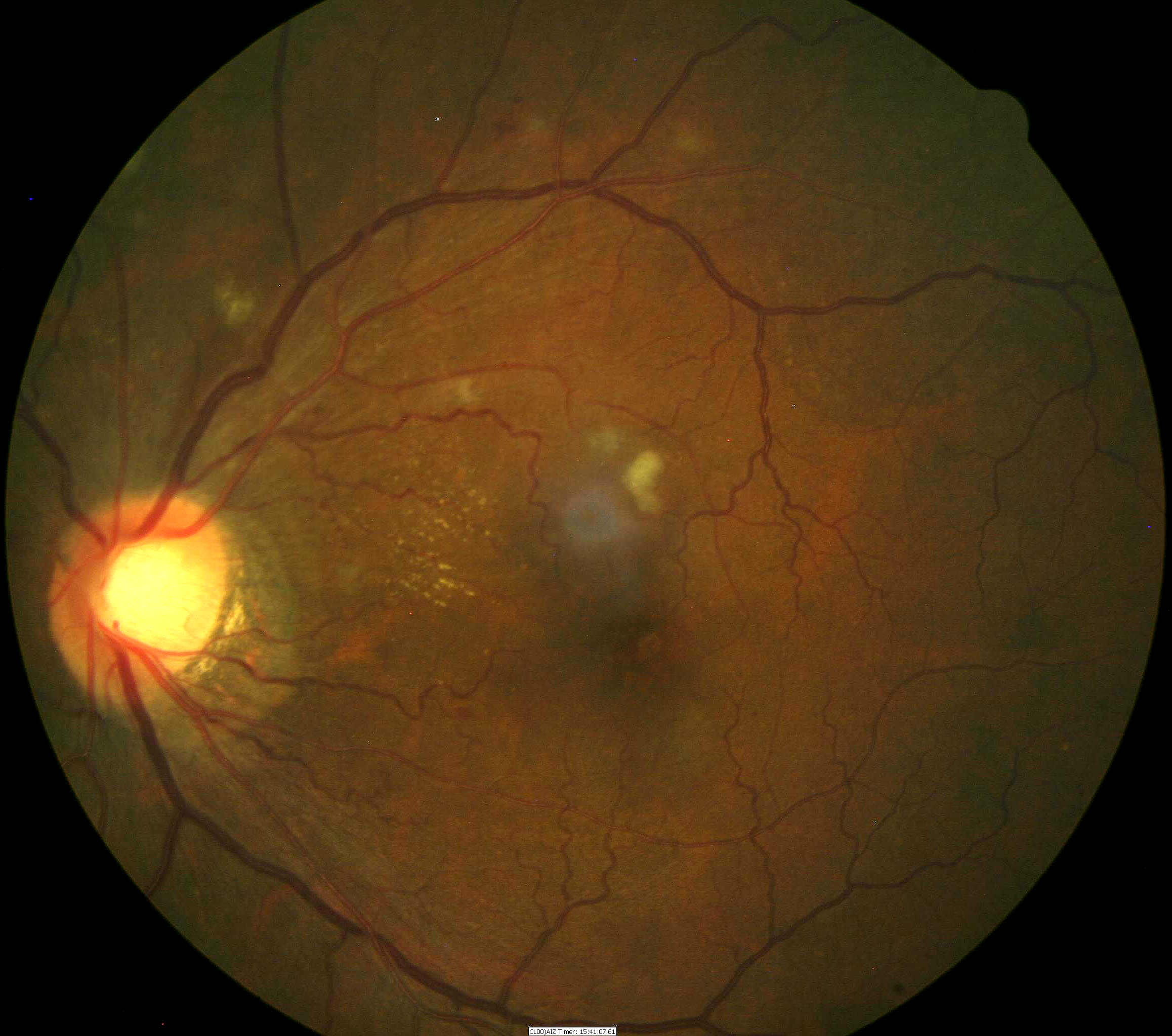
Diabetic Retinopathy after Laser Surgery
|
|
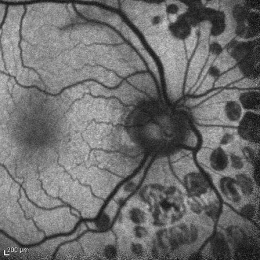 |
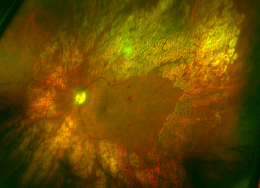
Fundus Autofluorescence Imaging
|
Retinal Scanning Laser
- To measure the microscopic anatomy of the retina and vitreoretinal interface
- To measure the effectiveness of therapy
- To help in determining the need for ongoing therapy
- To determine the safety of cessation of therapy
Visual Field Examination
- Used to assess visual function and determine the size of any associated visual field defects
- Visual field may be affected depending on the size and location of retinal hemorrhaging the extent of the visual field defect depends on size of macular edema
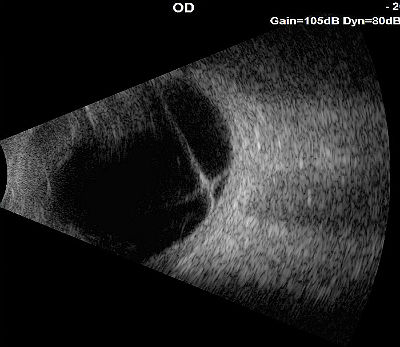
B-Scan Ophthalmic Ultrasound
- A two-dimensional ultrasonic scanning procedure used to produce cross-sectional images of the eye and orbit
- B-scan ophthalmic ultrasound can be used to assess internal structures of the eye when a vitreous hemorrhage prevents proper visualization and examination of the retina
- The test results are used to determine whether the retina is attached or detached
Diabetic retinopathy is classified into two types:
1. Non-proliferative diabetic retinopathy
- Mild
- Moderate
- Severe
 |
Mild Non-Proliferative Retinopathy
|
|
 |
Moderate Non-Proliferative Retinopathy
|
|
 |
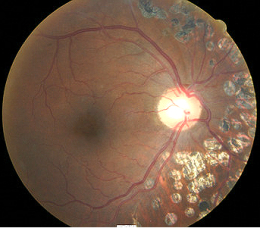
Severe Non-Proliferative Retinopathy
|
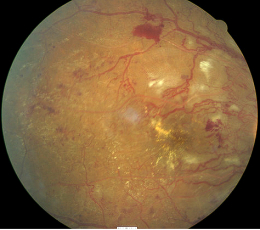
2. Proliferative Diabetic Retinopathy
- Definite neovascularization
- Preretinal hemorrhage
- Vitreous hemorrhage
- Fibrotic proliferation and vitreous scaffolding
 |
 |
|
 |
Proliferative Diabetic Retinopathy
|
This would include any eye diseases that produce changes in the retinal vasculature such as hemorrhages, microaneurysms, edema, and exudates.
 |
Hypertensive Retinopathy
|
|
 |
Retinal Venous Obstruction
|
|
 |
Retinal Telangectasia
|
|
 |
Leukemia
Ocular manifestations of leukemia can produce the following retinal vessel changes:
|
Palliative Treatment
- Change of diet, weight loss and incorporating exercise
- Managing any other medical conditions such as high blood pressure and high cholesterol can help reduce the risk
Pharmacologic Treatment
- Long term control of blood sugar either through oral medication or injection is important for preservation of vision, especially with no signs of diabetic retinopathy or the early stages of it
Surgical Treatment
 |
Laser Therapy
|
Intraocular Surgery
Vitrectomy — This procedure can is used to remove blood from the vitreous and scar tissue tugging on the retina.
1. Chous AP. The New Fundamentals of Diabetes. RevOptom. 2005 Sept 15; (9) 74-86.
2. Ajamian P. When To Refer A Diabetic Patient? RevOptom. 2003 May 15; (5) 86-88.
3. Wilkinson C. Classification of Diabetic Retinopathy: A Proposed International Clinical Disease Severity Grading Scale for Diabetic Retinopathy and Diabetic Macular Edema. Medscape/EMedicine. 2003 Sept 8. http://www.medscape.org/viewarticle/459913. Last accessed August 18, 2014.
4. Crisis. RevOptom. 2004 Sept 15; (9) 91-94.
5. Karpecki P. Nelson R. Extend Diabetes Care Beyond Retinopathy. 2004 Sept 15; (9) 100-112.
6. Chew R. The Optometrist’s Role in Diabetes. Optometric Management. 2007 June. http://www.optometricmanagement.com/articleviewer.aspx?articleid=100510. Last accessed August 18, 2014.
7. Gupta D. Systemic Hypertension. Optometric Management. 2007 June. http://www.optometricmanagement.com/articleviewer.aspx?articleid=100539. Last accessed August 18, 2014.
8. Gupta D. Screen for Diabetes. Optometric Management. 2007 June. http://www.optometricmanagement.com/articleviewer.aspx?articleID=71856. Last accessed August 18, 2014.
9. Gupta D. Managing Diabetes Medically. Optometric Management. 2004 Feb. http://www.optometricmanagement.com/articleviewer.aspx?articleID=70963. Last accessed August 18, 2014.
10. Practice Strategies: Diabetic Retinopathy Diagnosis On A New Scale. American Optometric Association. 2003 Nov; 74(11): 735-738.
362.01
Background diabetic retinopathy
92015
Refraction
92250
Fundus photography
92225
Extended ophthalmoscopy
92134
Macula OCT scan
92083
Visual field examination
92020
Gonioscopy
92275
Electroretinography
92283
Color vision examination
76512
B-Scan ophthalmic ultrasound
Occurrence
The prevalence of diabetic retinopathy among diabetic patients is 8.2% of the popular over the age of 40-years-old.
Distribution
- Diabetic retinopathy is not distributed evenly throughout the population
- Black Americans and Hispanics are more likely to develop diabetic retinopathy
Risk Factors
- Diabetes: Type 1 and type 2 diabetic patients are at risk
- Duration of diabetes: The longer patient has had diabetes the more likely they are to have some degree of diabetic retinopathy
- Poor control of blood sugar level
- Medical conditions such as high blood pressure and cholesterol increases the risk
- Pregnant women
- Smokers




 Print | Share
Print | Share