ICD-10 Diagnosis Code:
D33.3–Benign neoplasm of cranial nerves
Title
Benign Neoplasm of Cranial Nerves
Category
Benign Neoplasm Of Brain And Other Parts Of Nervous System
Description
Melanocytoma is a heavily pigmented tumor seen frequently in the optic nerve head but which can arise anywhere in the uvea.
Melanocytoma of the optic disc is a benign tumor caused by proliferation of the melanocytes normally found in the uvea and occassionally in the lamina cribrosa. It is characterized by the following clinical features:
- Optic disc melanocytoma is unilateral in 99% of patients
- Tumor is dark brown or black in color in 100% of patients
- Melanocytomas have feathery edges
- Mean tumor diameter is 2 mm and the mean thickness is 1 mm
- Mean age at initial diagnosis is 50-years-old
- On occassion, there is continuous involvement of the melanocytoma with the adjacent retina or choroid
- Usually no change in visual acuity
Histopathologically, melanocytoma of the optic disc is composed of heavily pigmented round to oval nevus cells with benign features. The cytoplasm of cells in melanocytoma are crowded with melanosomes. The tumor is usually stationary, but minor enlargement is seen in many patients. Malignant transformation is seen in 1-2% of patients.
Structural Damage to the Eye
- Afferent pupillary defects in 10-30% of patients
- Localized subretinal fluid in 10-14% of patients
- Patients may have pigment dispersion in the vitreous
- Tumor enlargement is present in 11% of patients by 5 years and 32% of patients in 10 years
- Enlargement can cause retinal nerve fiber layer defects
- Enlargement can cause compressive optic neuropathy, optic disc edema and optic atrophy
- Enlargement can cause retinal exudation
- Enlargement can cause compressive vascular problems (e.g., central retinal vein occlusion)
- Enlargement can cause tumor necrosis secondary to an inadequate blood supply
- Tumor necrosis can cause intraocular and orbital inflammation
Functional Damage to the Eye
- Afferent pupillary conduction defect may be present even with normal visual acuity
- Enlarged blind spot in 75% of patients
- Loss of visual acuity may occur secondary to a variety of mechanisms
The main goal of the diagnostic evaluation in a patient with melanocytoma of the optic nerve head is to accomplish the following:
- Evaluate tumor location, color, size and thickness
- Determine visual acuity
- Obtain baseline visual fields and fundus photographs
- Rule out malignant melanoma
Patient History
The symptoms of melanocytoma of the optic nerve head vary from no symptoms to severe visual impairment. Patients with a large tumor may have mild visual impairment and those with a progressive tumor may report decreased visual acuity over time.
Patients with melanocytoma of the optic disc may present with any of the following abnormal clinical signs or symptoms:
- Visual symptoms related to the melanocytoma are present in 24% of patients
- Ocular melanocytosis is present in 8% of patients
- Racial melanocytosis is present in 7% of patients
Pupillary Examination
- An afferent pupillary defect may be present in the affected eye
Clinical Appearance of the Retina
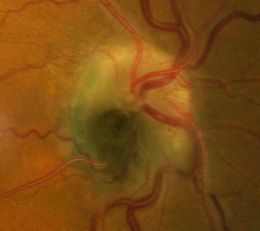
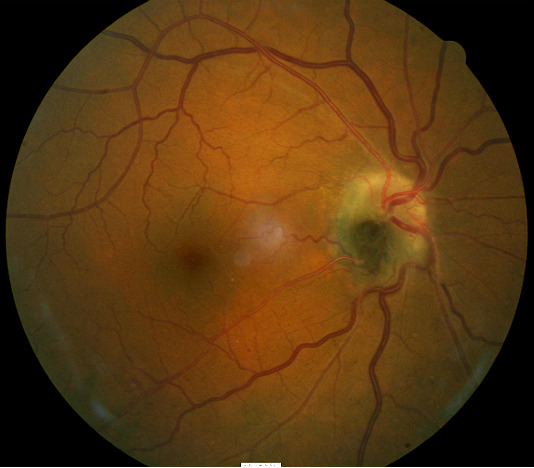
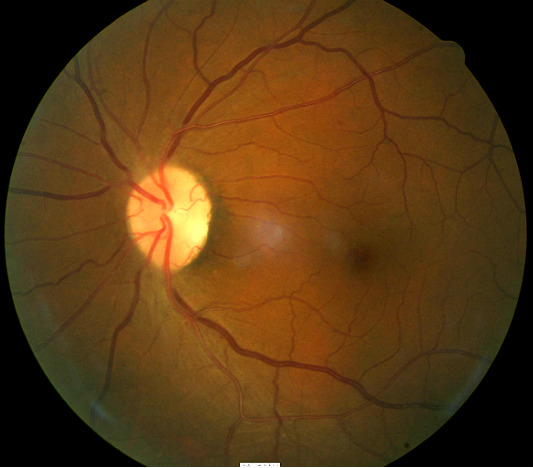
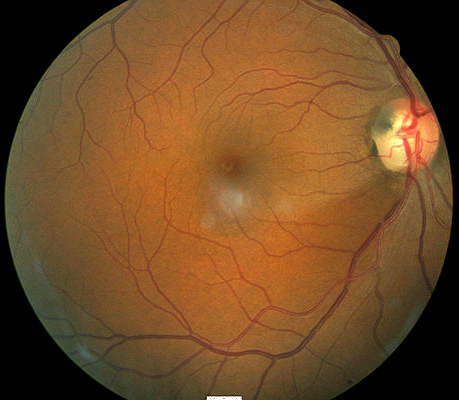
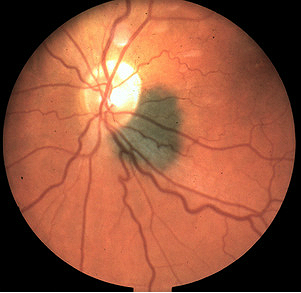
The following fundus images and diagnostic tests results are from a 53-year old dark-skinned black man.
The patient presented with a medium-sized black lesion sitting on the optic disc of the right eye. The mass occupies the inferotemporal quadrant of the optic nerve head and extends into the peripapillary area of the retinal nerve fiber layer.
- 20/20 visual acuity in the right eye
- 20/20 visual acuity in the left eye
 |
 |
DIAGNOSTIC TESTS
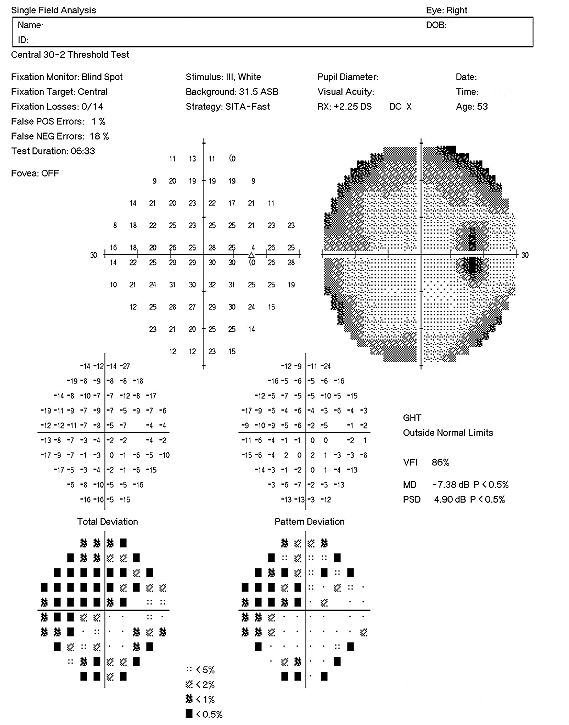
Visual Field Examination
- Enlarged blind spot secondary to melanocytoma in the right eye
- Inferior nasal arcuate scotoma in the left eye
- Superior visual field defects in both eyes
 |
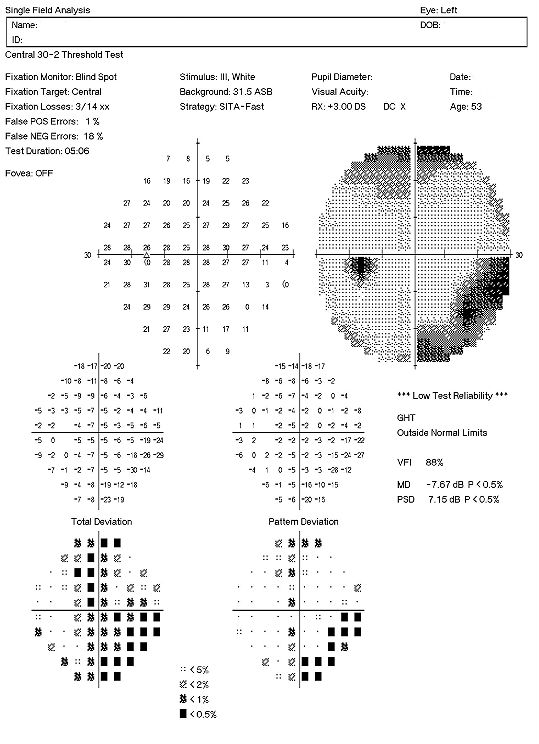 |
There are multiple visual field defects in each eye. Although the enlarged blind spot seen in the right eye is common in persons with melanocytoma of the optic nerve, these visual field abnormalities may also be caused by glaucoma. The coexistence of optic disc melanocytoma with possible glaucomatous optic neuropathy can be very challenging clinically because there is no specific means to differentiate whether the visual field defect is glaucoma-induced or related to the melanocytoma.
Retinal Laser Scan
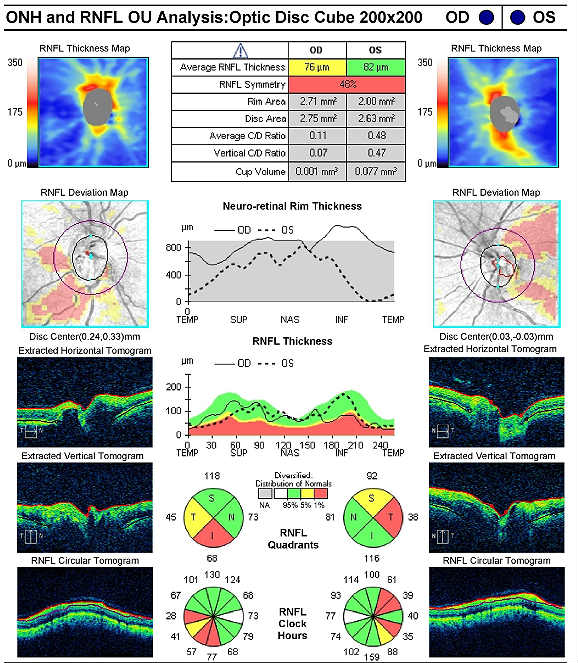 |
Right Eye
Left Eye
|
|
Right Eye
Left Eye
Both Eyes
|
 |
Optic disc melanocytomas can be classified by size and whether they are stationary or progressive
Stationary optic disc melanocytomas are characterized by the following clinical features:
|
 |
Malignant Melanoma of the Optic Nerve
Primary malignant melanoma of the optic nerve is very rare. However, because the clinical presentation is similar to melanocytoma in the early stage of the disease, it is important to differentiate between the two conditions. Significant differences between malignant melanoma and optic nerve melanocytoma include the following:
- Melanocytomas are dark and uniformly pigmented as opposed to the lighter color and varied pigmentation that characterizes malignant melanoma
- Melanocytomas usually present with normal visual acuity while malignant melanoma that involves the optic disc usually produces a severe decrease in visual acuity along with disc edema, retinal hemorrhages and retinal detachment
- Melanocytomas will show blocked fluorescence on fluorescein angiography while malignant melanomas often demonstrate altered areas of hyperfluorescence and hypofluorescence
 |
Choroidal Melanoma
|
|
 |
Congenital Hypertrophy of the Retinal Pigment
|
The goals of treating melanocytoma of the optic disc include the following:
- Document the location, color and size of the tumor with fundus photography
- Document the thickness of the lesion with B-scan ophthalmic ultrasound or extended ophthalmoscopy
- Rule out malignant melanoma
- Explain the benign condition of the lesion to the patient
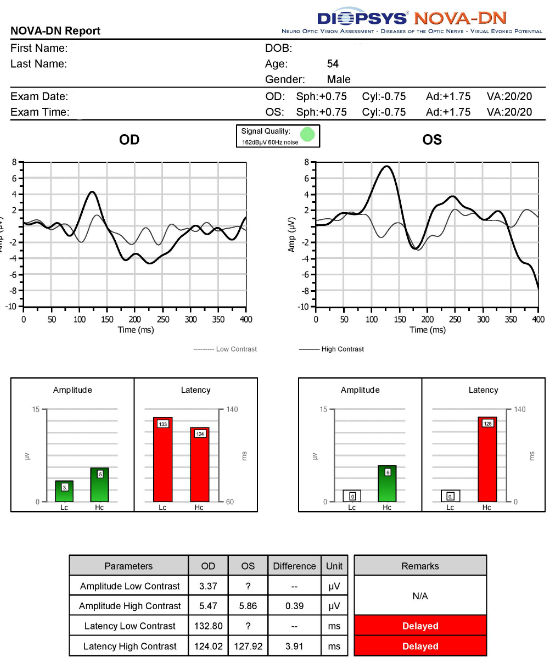
Monitor the tumor every 6 to 12 months for compression-related vasculopathy or malignant transformation with repeat visual field examination, serial fundus photography, B-scan ultrasound, extended ophthalmoscopy and/or visual evoked potential testing.
There is currently no treatment to prevent or stop optic nerve melanocytoma growth. Patients should be counseled about the risk of vision loss if the lesion increases in size.
Malignant transformation from optic disc melanocytoma to optic disc melanoma is associated with the following clinical signs:
- Rapid enlargement of the tumor mass
- Marked pigmentary changes of the tumor surface
- Profound decrease in visual acuity
When the optometrist or ophthalmologist is sure of the diagnosis, referral to a retinal specialist for the evaluation of optic disc melanocytoma is usually not necessary.
1. Parnes A, Im L, Wadhwa SD. The evaluation and management of optic disc melanocytoma. American Academy of Ophthalmology. http://www.aao.org/publications/eyenet/201105/pearls.cfm. Last accessed March 31, 2014.
2. Weidmayer S. Choroidal melanoma is a life sentence. RevOptom. Jan 15, 2012.
3. Optic nerve melanocytoma. Eye Cancer Foundation. http://www.eyecancer.com/conditions/38/optic-nerve-melanocytoma. Last accessed March 31, 2014.
4. Gahankari JR. Melanocytoma of the optic disc. Journal of Postgraduate Medicine. http://www.jpgmonline.com/article.asp?issn=0022-3859;year=1992;volume=38;issue=3;spage=135;epage=6;aulast=Gahankari. Last accessed March 31, 2014.
225.1
Benign neoplasm of cranial nerves
92083
Threshold visual field exam
92133
Retinal laser scan (RNFL)
95930
Visual evoked potential
92250
Fundus photography
92283
Color vision exam
76512
B-scan ultrasound
92225
Extended ophthalmoscopy




 Print | Share
Print | Share