ICD-10 Diagnosis Codes:
D31.31 — Benign neoplasm of right choroid
D31.32 — Benign neoplasm of left choroid
Title
Benign Neoplasm of Choroid
Category
Benign Neoplasm Of Eye
Description
A choroidal nevus is a benign melanocytic lesion of the posterior uveal tract.
Choroidal nevus is a benign tumor caused by proliferation of the melanocytes normally found in the uvea.
The lesion is characterized by the following clinical features:
- Usually no change in visual acuity
- Clearly defined margins
- Flat or slightly elevated
- Stable in size over time
- Overlying drusen
- Retinal pigment epithelial atrophy
- Hyperplasia
- Fibrous metaplasia
- Subretinal fluid
- Orange pigment
Structural Damge to the Eye
- None
- Subretinal and/or intraretinal fluid
- Cystoid retinal edema
- Choroidal neovascularization
Functional Damage to the Eye
- None
- Central and peripheral vision loss secondary to retinal complications
The main goal of the diagnostic evaluation in a patient with choroidal nevus is to accomplish the following:
- Evaluate tumor location, color, size and thickness
- Determine visual acuity
- Obtain baseline fundus photographs
- Rule out malignant choroidal melanoma
Patient History
The symptoms of choroidal nevus vary from no symptoms to severe visual impairment. Patients with a large nevus may have mild visual impairment secondary to retinal complications.
Patients with a choroidal nevus may present with any of the following abnormal clinical signs or symptoms:
- None
- Central and peripheral vision loss secondary to subretinal fluid
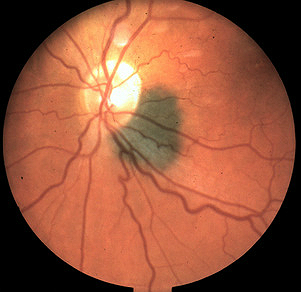
Clinical Appearance of the Retina
DIAGNOSTIC TESTS
Fundus Photography
- Document the size, shape, color, location and height of choroidal nevus
- Document associated clinical features of choroidal nevus
Retinal Laser Scan
- Document the presence or absence of subretinal fluid at the macula
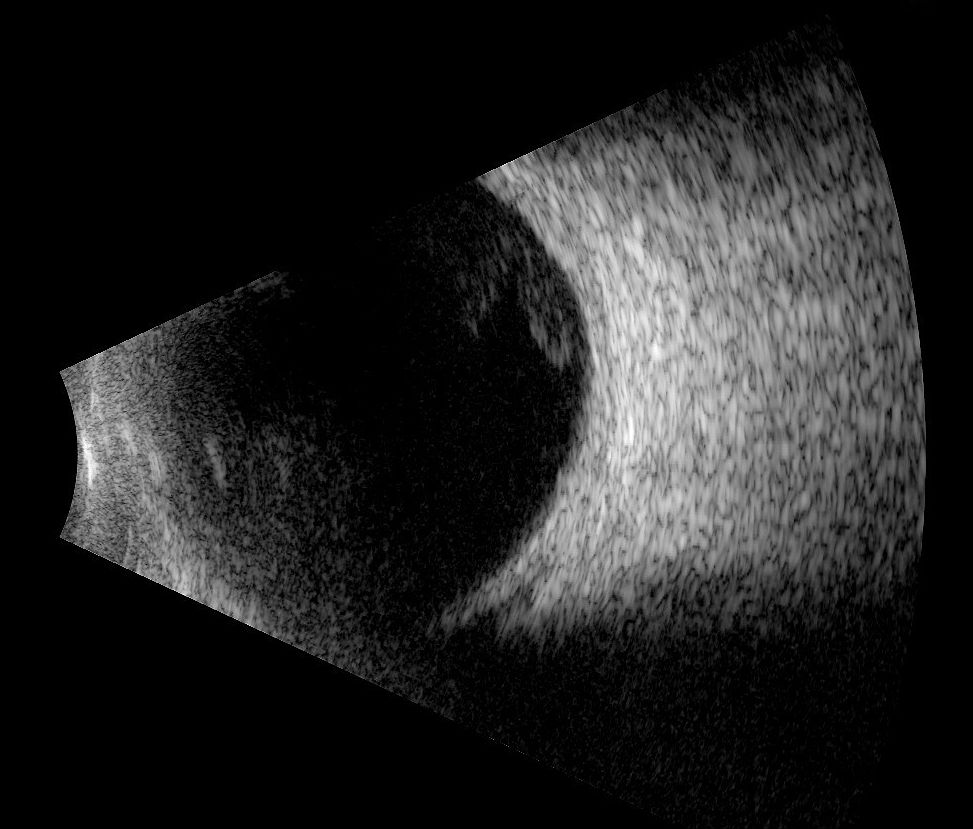
B-Scan Ophthalmic Ultrasound
- Document the presence or absence of ultrasound hollowness within the choroidal nevus
- Document the height of the choroidal nevus
- Document the presence or absence of choroidal tissue excavation
- Follow-up for at least 1.5 years may be necessary to differentiate between a choroidal nevus and a choroidal melanoma
A choroidal nevus may be pigmented or non-pigmented.
Choroidal Melanoma
Risk factors for identification of a small choroidal melanoma (when it might resemble a nevus), have been identified. Documented growth/change of a choroidal nevus over one to two years is a characteristic of malignant transformation.
The treatment of a benign choroidal nevus is determined by its risk of malignant transformation into a choroidal melanoma.
- Patients with no suspicious features require no treatment
- After the initial diagnosis, patients should be monitored twice during the first year
- Subsequently, annual surveillance examinations are recommended as long as the nevus remains stable
It is not common for a choroidal nevus to transform into a malignant melanoma. The annual rate of malignant transformation is estimated to be 1 in 8,845. The rate of malignant transformation increases with age and by age 80 the rate increases to 0.78%.
- A choroidal nevus that has one risk factor for growth has a 3% chance of growth at five years
- Patients with one or two risk factors should be examined every six months
- A choroidal nevus with three or more risk factors has a 50% chance of growth at five years and probably represents a small choroidal melanoma
1. Cheung A, Scott I, Murray T, Shields C. Distinguishing a Choroidal Nevus From a Coroidal Melanoma. American Academy of Ophthalmology. http://www.aao.org/publications/eyenet/201202/pearls.cfm. Last accessed June 6, 2014.
2. Zolotarev F, Turaka K, Shields C. SMall Choroidal Melanoma With All Eight Risk Factors for Growth. http://bmctoday.net/retinatoday/pdfs/1010RT_Oncology_Zolotarev.pdf. Last accessed June 6, 2014.
3. Reed K. Is It A Nevus Or Melanoma? Optometric Management. 2011 Sept. 1.http://www.optometricmanagement.com/articleviewer.aspx?articleID=106126. Last accessed June 7, 2014.
224.6
Benign neoplasm of choroid
92250
Fundus photography
92225
Extended ophthalmoscopy
76511
A-scan ultrasound
76512
B-scan ultrasound
92134
OCT scan of the macula
Occurrence
- The prevalence ranges from 4.6% to 7.9% in Caucasians
Distribution
- Men and women are affected equally
Risk Factors
- Caucasian ethnicity




 Print | Share
Print | Share