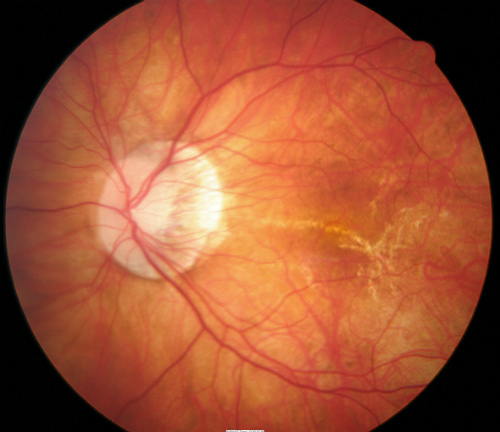
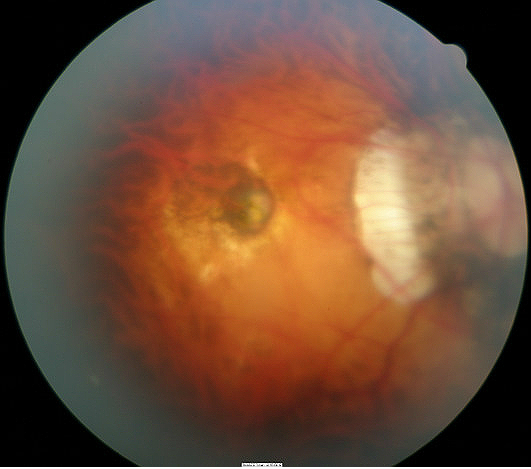
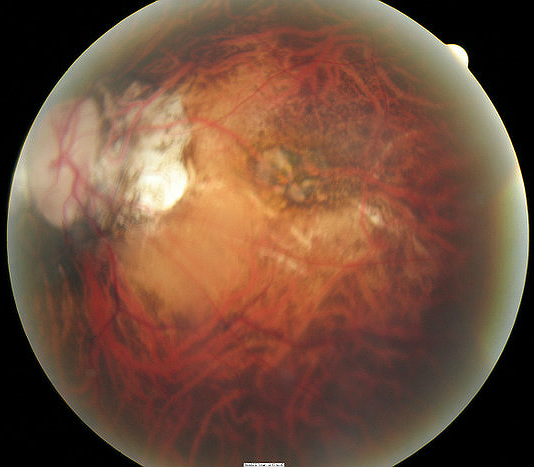
Patient with high myopia (-21.00 D) and
degenerative retinal changes
ICD-10 Diagnosis Codes:
H44.21–Degenerative myopia, right eye
H44.22–Degenerative myopia, left eye
H44.23–Degenerative myopia, bilateral
Title
Progressive High (degenerative) Myopia
Category
Disorders Of The Globe
Description
High myopia is defined as myopia greater than 6 diopters and an axial length of 26.5 mm while pathologic (degenerative) myopia will exhibit an axial length of 32.5 mm.
High myopia is defined as myopia greater than 6.00 diopters and an axial length > 26.5 mm, while pathologic (degenerative) myopia will exhibit an axial length > 32.5 mm.
Pathological myopes may present with any of the following abnormal signs:
- Decreased visual acuity
- An unusually large exophoria
- Strabismus (typically exotropia)
- Open-angle glaucoma
- Premature lenticular opacification
- Increased axial length
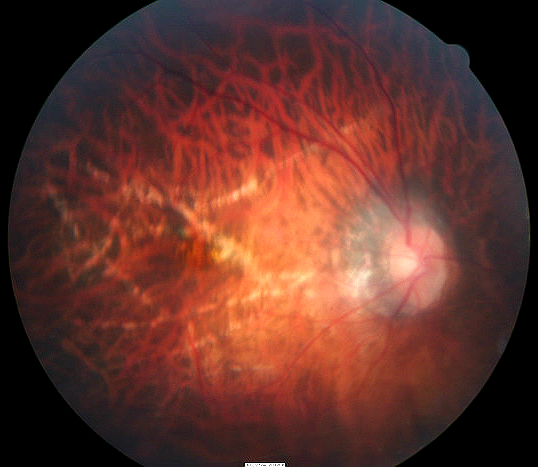
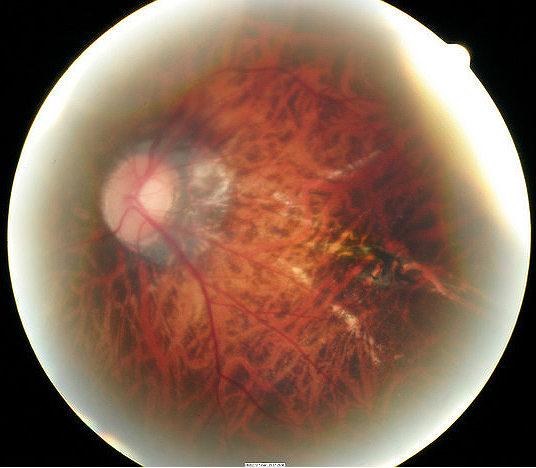
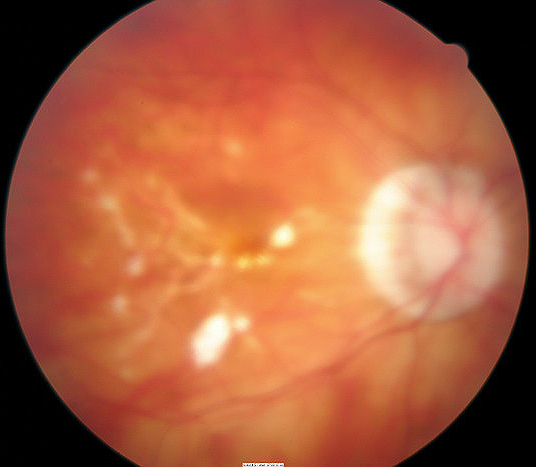
Internally the retina can have any of the following clinical features:
- A flat, obliquely inserted discs
- Posterior staphyloma
- Myopic crescent
- Patchy choroidal atrophy within the posterior pole
- Macular pigmentary abnormalities
- Vitreous syneresis
- Lacquer cracks or breaks in Bruch’s membrane with accompanying choroidal atrophy
- Subretinal neovascular membrane with overlying retinal pigment epithelial hyperplasia (Fuchs’ spot)
- Subretinal neovascularization without Fuchs’ spot (subretinal scarring, bleeding, exudate)
- Retinal breaks or detachments
Structural Damage to the Eye
- Patchy choroidal atrophy within the posterior pole
- Macular pigmentary abnormalities
- Vitreous syneresis
- Lacquer cracks or breaks in Bruch’s membrane with accompanying choroidal atrophy
- Subretinal neovascular membrane with overlying retinal pigment epithelial hyperplasia (Fuchs’ spot)
- Subretinal neovascularization without Fuchs’ spot (subretinal scarring, bleeding, exudate)
- Retinal breaks or detachments
- Separation of sensory retinal tissue to underlying retinal pigment epithelium and choroid due to holes, tears or breaks
- Accumulation of subretinal fluid in inappropriate places
- Traction from inflammatory or vascular fibrous membranes causes adhesions between the vitreous gel and the retina leading to detachments
Functional Damage to the Eye
- Decreased vision
- Increase chances of permanent vision loss if complications like retinal detachments occur then the following functional damage can seen
- Associated visual field defects and vision loss
- Sometimes visual acuity is affected depending on how close detachment is to the macula
- Visual distortions or disturbances noted
- Increase in floaters or flashes of light severely affects patients ability to function
The main goal of the diagnostic evaluation of a patient with high degenerative myopia is to accomplish the following:
- Determine the extend of the structural damage in the retina
- Isolate any potential risk for retinal detachment
- Determine a monitoring or treatment regimen
Patient History
Most patients with high degenerative myopia are asymptomatic unless they experience a complication such as a retinal detachment then they will experience the following symptoms:
- Visual disturbances (such as flashes and/or floaters)
- Black curtain or film cover their visual field
- Sudden vision loss
Clinicial Appearance of the Retina
- Usually bilateral
- Flat, obliquely inserted discs
- Posterior staphyloma and/or a myopic crescent present
- Look for patchy choroidal atrophy within the posterior pole
- Breaks in Bruch’s membrane with accompanying choroidal atrophy known as lacquer cracks may be present
- Look for choroidal neovascular membrane (CNVM) with overlying retinal pigment epithelial hyperplasia (Fuch’s spot)
- Look for subretinal neovascularization without Fuch’s spot (subretinal scarring, bleeding, and exudate)
- Vitreous syneresis
- Retinal breaks or detachments
 |
 |
DIAGNOSTIC TESTS
Refraction
- Measurement of visual function / visual acuity
Extended Ophthalmoscopy
- Evaluate optic disc morphology
- Document abnormal structural changes to the optic disc
- Evaluate for any abnormal retinal thinning, tears or detachments
- Evaluate for choroidal neovascular membrane (CNVM)
Fundus Photography
- Evaluate abnormal retinal and macular changes
 |
 |
Retinal Scanning Laser
- Attenuation of the retinal nerve fiber layer
- Excavation of the optic disc
A-Scan and/or B-Scan Ophthalmic Ultrasound
- Used to determine axial length and confirm posterior staphyloma
Developmental Stage
There are two stages of degenerative myopia, and the first is call the developmental stage. This early stage of the disease is characterized by abnormal axial lengthening and then followed by damage from vascular alterations.
 |
 |
Degenerative Stage
- Elongation of the globe, known as posterior staphyloma, occurs and results from scleral thinning
- This progressive scleral ectasia can form in the posterior pole (disc and macula), inferiorly, nasally or in multiple, complex patterns
- Lacquer cracks or breaks in Bruch’s membrane with accompanying choroidal atrophy are formed – these dehiscences results in an increased risk for choroidal neovascularization
 |
 |
Macular Degeneration
The retina may develop CNVM and the macular has a similar appearance, but with macular degeneration drusen is present and the myopic features from degenerative myopia are absent.
Tilted Disc
Patient with a tilted disc will have a scleral crescent that is often inferonasal and usually there is an irregular vascular pattern as the vessels emerge from the disc. There is often a corresponding visual field defect to the fundus ectasia. Bilateral cases are common.
Ocular Histoplasmosis
CNVM may develop and have a peripapillary scar. Round choroidal scars that look like punched-out lesions are seen throughout the fundus.
Toxoplasmosis
The retina will have distinct well-circumscribed chorioretinal scars that do not typically develop CNVM and the active form of the disease shows retinitis and vitritis.
Coloboma
These are large abnormal appearing optic disc as a result of incomplete closure of the embryonic fissure. They are located inferonasally on the retina.
There is no treatment that regresses or stops the progression of the staphyloma in degenerative myopia.
Pharmacological Therapy
- Atropine is experimentally used in children to ease the stresses and strains from accommodation
Corrective Ophthalmic Lens Therapy and Surgery Options
- Patient’s refractive error can be corrected with glasses. Recommend polycarbonate for greater protection, plastic (zylonite) frames to mask increased edge thickness of lens with special edge polishing and buffing to improve lens cosmetics.
- Patient’s refractive error can be corrected with contacts (soft and rigid gas permeable lenses). Soft contact lens offer comfort and convenience, but closely monitor for hypoxia if not using silicone-hydrogel lenses. Rigid gas permeable lenses offer good optics and physiological health (a minus lenticular design may be appropriate to minimize complications and discomfort of edge thickness)
- LASIK is not recommended for patients with degenerative myopia. Intraocular lens implantation may be an alternative to refractive surgery
Preventative Therapy
- Avoid dangerous circumstances and activities such as contact sports or activities that jolt the body since it can increase the chances of a retinal detachment
Treating the complications that can arise from degenerative myopia
- Routinely monitor patients for choroidal neovascularization membrane (CNVM) formation and retinal detachments
- Extrafoveal or juxtafoveal CNVM can be treated with laser photocoagulation
- Symptomatic retinal breaks can be treated with laser photocoagulation, cryotherapy or scleral buckling surgery
1. Pathological Myopia and Posterior Staphyloma. Handbook of Ocular Disease Management. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1311542/. Last accessed August 17, 2014.
2. Roberts D. Degenerative Myopia. Nov 2007. http://lowvision.preventblindness.org/eye-conditions/degenerative-myopia. Last accessed August 17, 2014.
3. Kabat A. Sowka J. Monitor Progressive Myopia. RevOptom. 18 Aug 2010. http://www.reviewofoptometry.com/content/c/22052/. Last accessed August 17, 2014.
360.21
Progressive high (degenerative) myopia
76511
A-scan ultrasound
76512
B-scan ultrasound
92015
Refraction
92225
Extended ophthalmoscopy
92250
Fundus photography
92083
Visual field examination
92283
Color vision examination
92275
Electroretinography
Occurrence
The incidence of degenerative myopia is almost 2% of the population.
Distribution
- Degenerative myopia is not distributed evenly throughout the population
- Patients of Chinese, Japanese, Jewish and Arabic decent are at a higher risk
Risk Factors
- Females are two times more likely to have degenerative myopia
- Marfan’s syndrome
- Retinopathy of prematurity
- Ehler’s-Danlos syndrome
- Stickler’s syndrome
- Albinism




 Print | Share
Print | Share