Vitreous degeneration
ICD-10 Diagnosis Codes:
H43.811–Vitreous degeneration,right eye
H43.812–Vitreous degeneration,left eye
H43.813–Vitreous degeneration,bilateral
Title
Vitreous Degeneration
Category
Disorders Of The Vitreous
Description
The vitreous is a gell-like substance that helps the eye maintain a round shape. Vitreous degeneration or vitreous syneresis is a natural progression of the vitreous becoming less transparent. As the vitreous breaks down the patient experiences black shadow-like “dots” in their field of view.
The eye’s interior is filled with vitreous, a gel-like substance that helps the eye maintain a round shape. The vitreous is made up of collagen fibrils and glycoaminoglycans, supported by hyaluronic acid molecules. These millions of fine fibers are intertwined within the vitreous and are attached to the surface of the retina around the ora serrata and throughout most of the posterior pole. The attachment at the ora is very strong while the attachment throughout the posterior pole is relatively weak except around the optic nerve and somewhat at the macula. With aging, there is a decrease in hyaluronic acid molecules supporting the collagen. As a result, the vitreous slowly shrinks and these fine collagen fibers pull on the retinal surface. Usually the fibers break, allowing the vitreous to separate and shrink from the retina resulting in a posterior vitreous detachment without any complications. Sometimes the breaks can result in rhegmatogenous retinal detachments if the vitreous strands pull off retinal tissue as well during the posterior vitreous detachment.
Structural Damage to the Eye
- Shrinkage of the vitreous with age
- Vitreoretinal adhesions can cause a tear in the sensory retina resulting in a Rhegmatogenous retinal attachments, macular tear or macular hole formation through a process of vitreomacular traction syndrome (VMT)
Functional Damage to the Eye
- Although visual acuity is usually not affected in an asymptomatic posterior vitreous detachment, patients describe their vision as, “not as clear or sharp” if the vitreous detachment has not completely settled
- If the vitreous detachment is also associated with a macular tear or rhegmatogenous retinal attachments, visual acuity and/or visual field may be affected
- Visual distortions or disturbances noted can be a result of macular tear or rhegmatogenous retinal attachments.
- Increase in floaters as a result of vitreous shrinkage
- Flashes of light reported by patients can be a result of the vitreoretinal adhesions not completely separating from each other. The presence of symptomatic flashes of light demands careful attention to examination of the vitreo-retinal interface
The main goal of the diagnostic evaluation is to determine the following:
- Evaluate any associated structural damage such as retinal detachments or VMT
- Identify and exclude differential diagnosis
- Prescribe a monitoring program or treatment program if a retinal detachment is also present
Patient History
Patients present with the following signs:
- Sudden onset of visual distortions or visual disturbances are present
- Often complain of “specks of dust or string-like” shadows in their field of view
- Patients report “cleaning their glasses but the specks don’t go away”
Although uncommon, vitreous degeneration or detachment can be associated with a break in an anterior retinal vessel, creating small pre-retinal hemorrhages. If the blood breaks through the internal limiting membrane, a vitreous hemorrhage will result. If the vitreous hemorrhage is significant, patients will not have cobweb and floater symptoms but instead will report significant reduction in vision.
Another uncommon sign is pigment cells in the anterior vitreous. These are much smaller and far more anterior than normal floaters.
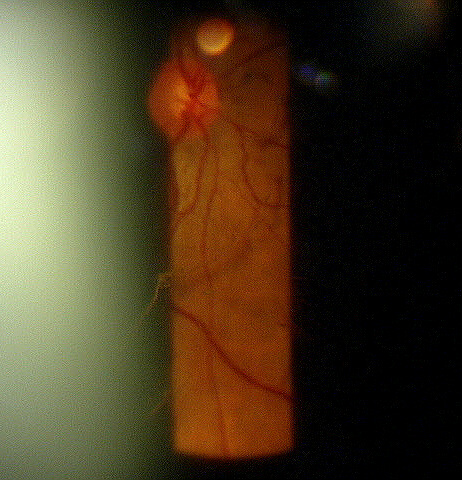 |
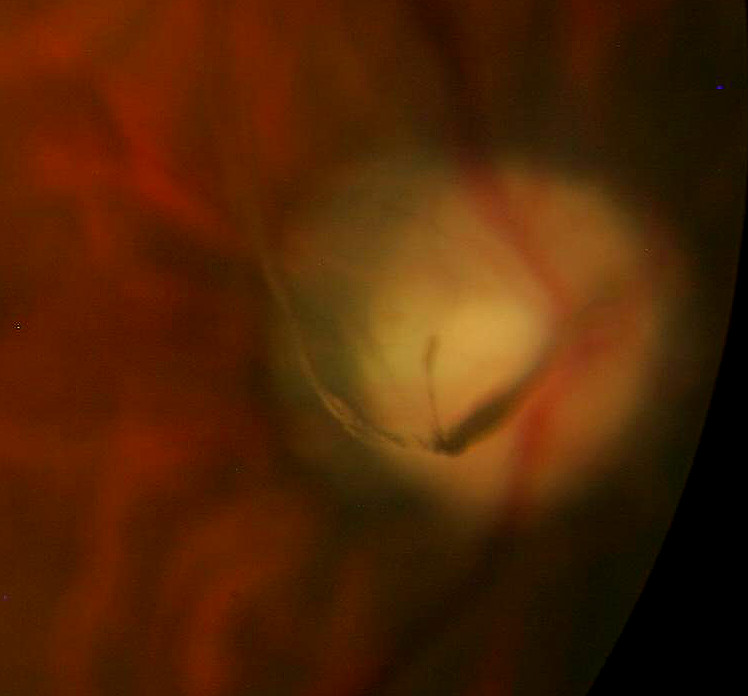
Clinical Appearance of the Retina
|
DIAGNOSTIC TESTS
The following tests can assist in the diagnosis and confirmation of posterior vitreous detachment:
Refraction
- Measurement of visual function / visual acuity
B-Scan Ophthalmic Ultrasound
- If the retina cannot be visualized due to corneal changes, cataracts or hemorrhages, it is necessary to use ultrasound to differentiate between retinal detachments versus vitreous detachment
Extended Ophthalmoscopy
- Can help with more thoroughly documenting holes, tears or breaks in the retina, pigment cells or blood seen in the posterior pole or peripheral retina
- Helps document the extent of any remaining vitreous adhesion to the retina
In general, vitreous degeneration and resultant vitreous detachments can be classified as complicated or uncomplicated. Uncomplicated posterior vitreous detachments typically involve a complete and total break of the vitreous from the posterior pole with no tractional complications at the ora base.
Complicated posterior vitreous detachments would include vitreous degeneration that carries moderate to signficant risk of additional retinal traction at the ora or macula. Complicated posterior vitreous detachments would include visible traction at the ora and vitreo-macular traction (VMT). VMT with an incomplete vitreous detachment from the optic nerve carries less risk of tractional complications in the macula as the vitreous is still “anchored” at the optic nerve.
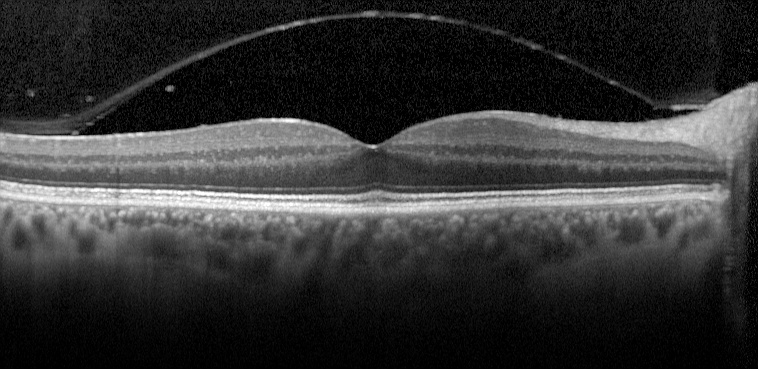 |
Rhegmatogenous retinal detachments and less commonly macular holes can occur as a result of vitroretinal adhesions causing a tear in the sensory retina |
Uncomplicated vitreous detachments are common, especially at the posterior pole. There are few retinal complications that mimick the patient symptoms and retinal signs associated with vitreous degeneration. These include:
Migraine
- Patients with transient vascular insufficiency during a migraine event can experience various photopsias including perceptions of cobwebs, zig-zag lines and flashes of light.
- Migraine events have characteristic presentations and should be easily distinguished from symptoms from vitreous degeneration.
Vitritis
- Vitreous cells may be difficult to distinguish from pigment cells.
- Vitreous cells from inflammation are typically not pigmented and will be seen throughout the vitreous whereas pigmented cells are confined to the anterior vitreous.
- It is very important to differentiate whether cells in the vitreous are from an inflammatory process or non-inflammatory pigment (RPE) origin.
- Inflammatory vitreous cells are most commonly associated with systemic or local retinal inflammatory conditions.
- True pigment cells, especially seen with vitreous blood in patients with symptomatic vitreous degeneration is highly indicative of a peripheral retinal break.
Treatment depends on whether the patient is symptomatic and if there is an associated macular or retinal detachment.
Symtomatic after posterior vitreous detachment WITH macular or retinal tears/detachments
In most all cases, retinal tears require immediate treatment aimed at repairing the tear or attachment.
Surgery for Retinal Tears For retinal holes or tears that have not advanced to a retinal detachment, preventative measure can be taken with the following procedures:
- Laser surgery (photocoagulation): A laser is used to make burn marks around the retinal hole or tear to encourage scarring. This scarring welds together the underlying tissue and prevents the tear from developing into a retinal detachment.
- Freezing (cryopexy): A freezing probe applied to the outer surface of the eye is used to freeze the retina around the retinal tear. This technique freezes the area around the hole, leaving a scar to secure the retina to the eye wall. It is generally used for hard-to-reach tears.
- Significant vitreo-macular traction with impending macular hole formation can be considered for newer vitreolysis therapy with intravitreal Plasmogin.
Surgery for Retinal Detachments
If a retinal attachment has occurred the following procedures are utilized. The type, size and location of any retinal detachment determines the technique used.
- Pneumatic retinopexy: This procedure is used for an uncomplicated detachment with the tear located in the upper region of the retina. Cryopexy is used to treat the retinal tear first. A bubble of expandable gas is injected into the vitreous cavity. Over the course of a few days, the gas bubble expands sealing the retinal tear by pushing against it and the detached area surrounding the tear. Since no new fluid is passing through the retinal tear, the previously accumulated fluid is absorbed, and the retina is able to reattach itself to the back wall of your eye. The gas eventually disappears on its own in several weeks.
- Scleral buckling: This is the most common technique for repairing retinal detachment. Cryopexy is used to treat the retinal tear first. Then a small piece of silicone sponge or silicone rubber is attached to the sclera over the affected area. The silicone material indents the wall of the eye, therefore, creating a buckling effect and reducing traction of the vitreous on the retina. The silicone material is stitched to the outer surface of the sclera. A small cut in the sclera can be made to drain any fluid collected under the detached retina before tying the sutures to hold the buckle in place. The scleral buckle remains in place for the rest of the patient’s life, although the purpose of the buckle ends shortly after the initial surgery.
- Vitrectomy: Sometimes removing part of the vitreous is necessary when vitreous clouding prevents a view of the detached retina or retinal scarring limits the effectiveness of pneumatic retinopexy or scleral buckling. Scar tissues or opaque areas of the vitreous are removed, while the volume of removed tissue is balanced with salt solution to maintain the normal pressure and shape of the eye. After the vitrectomy, the other various techniques are used to repair the retinal tear or detachment.
Asymptomatic posterior vitreous detachment WITH retinal tears/detachment or retinal degeneration (lattice degeneration)
- Depending on the size, location and extend of the tear/detachment or degeneration, treatment is simply monitoring the condition or utilizing the same techniques describe for symptomatic patients are utilized
Symptomatic posterior vitreous detachment with NO macular or retinal tears/detachments
- Educate patient on the timeline for symptoms to resolve and monitor every 1 to 6 weeks depending on symptoms, risk factors and vitreous traction
Asymptomatic posterior vitreous detachment with NO macular or retinal tears/detachment or retinal degeneration (lattice degeneration)
- After initial visit, monitor in 6 weeks, then annually
1. Posterior Vitreous Detachment. http://www.webmd.com/eye-health/tc/posterior-vitreous-detachment-topic-overview. Last accessed July 3, 2014.
379.21
Vitreous degeneration
92015
Refraction
92225
Extended ophthalmoscopy
92134
Macula OCT scan
76512
Ophthalmic ultrasound
Occurrence
The prevalence of posterior vitreous detachment is 4% of the population over the age of 50.
Distribution
- Posterior vitreous detachment is not distributed evenly throughout the population
- More common in people over the age of 50
Risk Factors
- Age
- High myopia
- Previous eye surgery such as cataract removal
- Previous severe eye injury or trauma
- Weak areas in the peripheral retina




 Print | Share
Print | Share