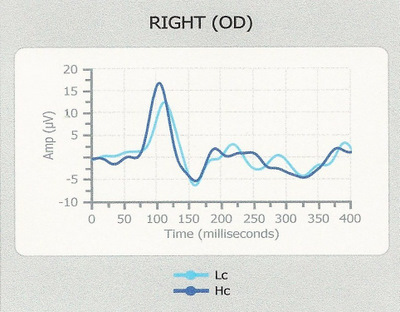
Normal VEP waveform response in patient
reporting decreased vision
ICD-10 Diagnosis Code:
F44.6 — Conversion disorder with sensory symptom or deficit
Title
Conversion Disorder
Category
Anxiety Dissociative And Somatoform Disorders
Description
Conversion disorder is a condition in which a person has the loss of one or more bodily functions (e.g., blindness) that cannot be explained by physical examination.
Conversion disorder is a mental disease that presents as a loss of physical function suggestive of a physical disorder.
Conversion symptoms are presumed to result from an unconscious process and conversion disorder is presumed to be the expression of an underlying psychological conflict or need. Optometrists and ophthalmologists must consider a diagnosis of conversion disorder when they examine patients who report decreased vision that cannot be explained by ocular examination.
Clinical symptoms of a conversion disorder include the loss of one or more physical functions, such as:
- Weakness
- Blindness
- Numbness
- Gait disturbances
- Paralysis
- Inability to speak
Visual symptoms of conversion disorder include the following:
- Monocular diplopia
- Triplopia
- Visual field defects
- Tunnel vision
- Bilateral blindness
Conversion disorder symptoms may occur because of psychological conflict and stress. It is important to understand that in true conversion disorder, patients are not making their symptoms up. Some doctors falsly believe that conversion disorder is not a real condition, and may tell patients that the problem is all in their head. However, these conditions are real to the patient. They cause stress, anxiety and disability.
People are more at risk for a conversion disorder if they have any of the following:
- Medical illness
- Dissociative disorder
- Personality disorder
Structural Damage to the Eye
- None
Functional Damage to the Eye
- None
The main goal of the diagnostic evaluation in a patient with conversion disorder is to accomplish the following:
- Exclude neurologic disease
- Exclude feigning (i.e., malingering)
- Determine a psychological mechanism
Patient History
- The symptoms of conversion disorder usually encountered by optometrists and ophtahlmologists involve decreased vision.
- The doctor must exclude neurological disease through ocular examination and appropriate diagnostic tests.
- To exclude feigning, the doctor must try to determine if the patient is intentionally trying to be deceptive.
- To determine a psychological mechanism, the doctor must believe that preceding stressors or conflicts are associated with the development of the condition.
Clinical Appearance of the Eye
- Normal cornea
- Normal crystalline lens
- Normal retina
DIAGNOSTIC TESTS
Refraction
- Subjective refraction evaluates the function of the complete visual system
- This test can be very unreliable in patients with conversion disorder
Visual Field Examination
- Threshold and/or supathreshold testing evaluates the function of the complete visual system
- Test results often reveal non-specific visual field defects
- High percentage false negatives generally invalidates any value in the findings.
- Subjective visual field testing can be very unreliable in patients with conversion disorder
56-year-old black man with non-specific visual field defects and unreliable test results.
 |
 |
Retinal Laser Scan
- Scanning lasers evaluate the structure of the retina, macula, and optic nerve
- In patients without true ocular or neurological disease, retinal laser scans will usually be normal
- Test results often do not suggest an etilogy for the patient’s symptoms of decreased vision
- Retinal imaging is usually very reliable in cooperative patients
Visual Evoked Potentials
- VEP testing evaluates the function of the complete visual system
- Normal VEP test results suggest the absence of a clinically significant neurologic disease affecting the visual pathways
- VEP testing is usually reliable in cooperative patients and even in somewhat uncooperative patients
- As long as the patient fixates the target, the test is almost impossible to “fake”
 |
VEPs Generate by a Diopsys NOVA-DN Testing Device
|
There is no classification system in place for conversion disorder. According to the Diagnostic and Statistical Manual of Mental Disorders of the American Psychiatric Association, Fourth Edition, Text Revision (DSM-IV-TR), conversion disorder is classified as one of the somatoform disorders. Other diseases in this category include hypochondriasis and body dysmorphic disorder.
Neurologic Disease
Look for evidence of a sensory function deficit that can explain the symptoms reported by the patient. Because it is fairly common for patients with neurologic disease to also have conversion disorder, the differential diagnosis may involve how much of the patient’s problem is due to conversion and how much is due to organic disease.
Ocular Disease
Look for evidence of a structural abnormality in the eye that can explain the symptoms reported by the patient.
Malingering
This condition refers to fabricating or exaggerating the symptoms of decreased vision for a variety of motives. Malingering is different from somatoform or dissociative disorders because the patient is trying to achieve some type of secondary gain from the behavior. Failure to diagnose malingering imposes a burden on the health care system, just as false attribution of malingering imposes a degree of suffering on patients who have true organic disease. To deliver the highest quality care, optometrists and ophthalmologists must either get the patient to confess to making up symptoms or prove deception is some other aspect of the examination.
Malingering should be suspected if any combination of the following are present:
- The presence of Antisocial Personality Disorder
- Significant discrepancy between the patient’s claimed loss of vision and the objective examination findings
- Lack of cooperation during diagnostic testing
- Lack of compliance with a prescribed treatment program
- A medicolegal context of the presentation
Malingering can often be identified by simply noting the patients response to tangent screen testing at two different distances. Although a simple test, the result can be very diagnostic.
Although there is little evidence-based treatment for conversion disorder, the primary goal is to treat patients as if their symptoms have an organic origin.
- If necessary, consultation with an outpatient psychiatric clinic may be required
- If true conversion disorder is suspected, this disease falls outside the realm of primary eye care disease and consultation with a neurologist or psychiatrist is warranted. For the sake of good medical care and the health care system, it is imperative that malingering be identified and not unduly drug through a series of testing and specialty consultations.
- Suggestive therapy may be an effective short-term treatment (i.e., an authoritative, not confrontive, pronouncement that “this problem usually goes away in a few weeks” is often successful, especially with children)
- Treatment of depression or anxiety if present
- Drug therapy has not proven reliable in treating conversion disorder
1. U.S. National Library of Medicine. Conversion disorder. Available at http://www.nlm.nih.gov/medlineplus/ency/article/000954.htm. Accessed March 3, 2014.
2. Medscape. Conversion disorder in emergency medicine. Available at http://emedicine.medscape.com/article/805361-overview. Accessed March 3, 2014.
300.11
Conversion disorder
92015
Refraction
92083
Threshold visual field exam
92133
Retinal laser scan (RNFL)
92134
Retinal laser scan (macula)
92275
Electroretinography
95930
Visual evoked potential
Occurrence
- The rate of conversion disorder averages about 16 persons per 100,000 per year
- Disease rates are higher in lower socio-economic groups, rural areas, and in neurological settings
- The condition is rare in children under 10 years old and in the elderly
- Most patients are affected in their mid-to-late 30s
Distribution
Conversion disorder is not evenly distributed in the population.
Risk Factors
- Females are affected 2-6x more often than men
- Pre-existing mental disease




 Print | Share
Print | Share