ICD-10 Diagnosis Codes:
S05.01XA–Corneal abrasion, initial encounter, right eye
S05.01XD–Subsequent encounter, right eye
S05.01XS–Sequela of corneal abrasion, right eye
S05.02XA–Corneal abrasion, initial encounter, left eye
S05.02XD–Subsequent encounter, left eye
S05.02XS–Sequela of corneal abrasion, left eye
Title
Superficial Injury of Cornea
Category
Superficial Injury Of Eye And Adnexa
Description
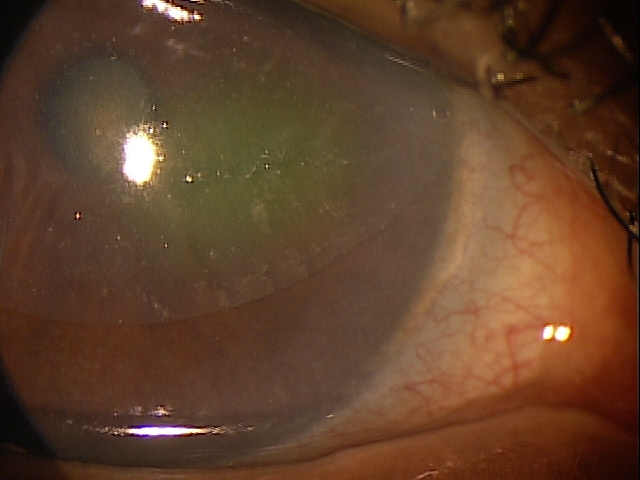
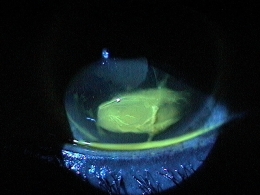
A corneal abrasion is a scratch or scrape of the cornea. It can result from foreign bodies, contact lenses, chemicals, or anything causing mechanical trauma such as fingernails, hair brushes, vegetative matter, dust, metal shards or projectile objects.
Structural Damage to the Eye
- Damage of the cornea at a superficial level — break does not involve Bowman’s membrane
- Damage of the corneal at a deeper level — break penetrates Bowman’s membrane, but does not rupture Descemet’s membrane
Functional Damage to the Eye
- Blurred vision as a result of the compromised cornea
- Corneal edema can result from the insult to the cornea depending on the level of damage
The main goal of the diagnostic evaluation of a patient with corneal abrasion is to accomplish the following:
- Assess the amount of structural damage to the cornea
- Reduce patients symptoms
- Manage pain accordingly
- Prevent further damage to the cornea
- Reduce re-occurrence of damage to the cornea during the healing process
Patient History
Patients with corneal abrasion may present with any of the following clinical symptoms:
- Acute pain
- Tearing
- Photophobia
- Blurred vision
- Foreign body sensation
- Blepharospasm
- Pain with eye movements
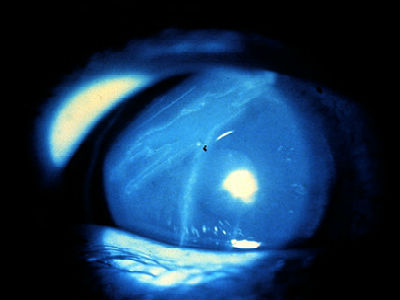
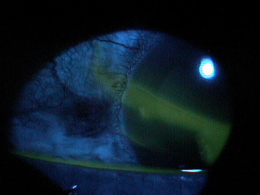
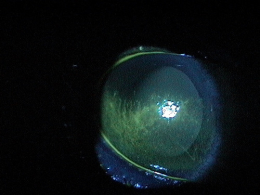
External Ocular Examination with Biomicroscopy
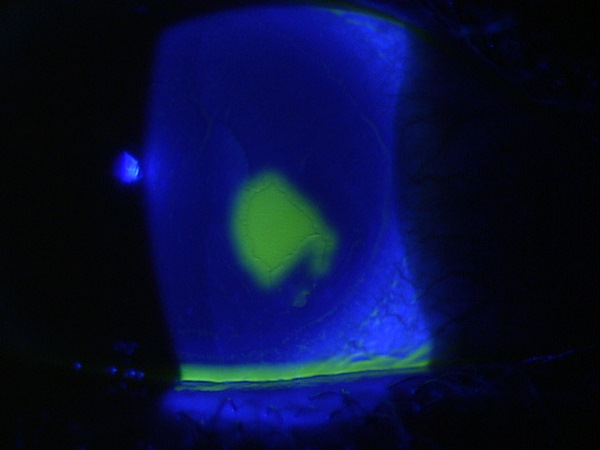
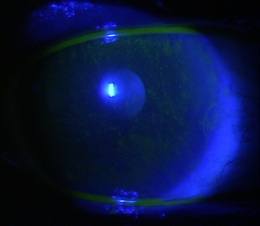
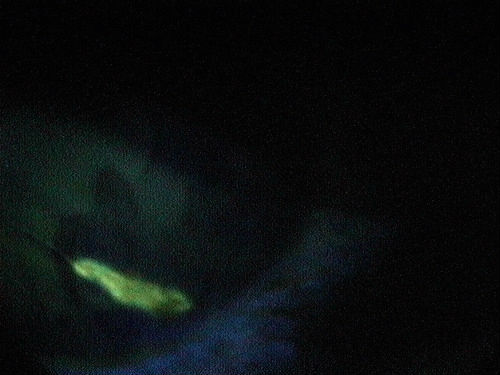
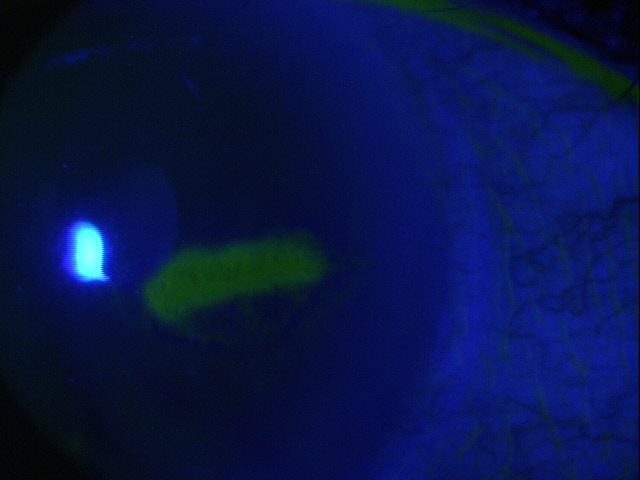
- Measure the size of the abrasion by using fluorescein dye
- Evaluate the anterior chamber for signs of ocular inflammation (e.g., cells and flare)
- Rule out penetrating trauma
DIAGNOSTIC TESTS
External Ocular Photography
- Used to document degree of corneal damage
Recurrent Corneal Erosions
- The symptoms of pain, discomfort and photophobia are the same; however the etiology of the corneal damage is very different (the case history is very important in differentiating the two)
- Corneal abrasions are usually caused by foreign bodies, contact lenses, chemicals, or some form of trauma
- Recurrent corneal erosion happen from rubbing their eyes or opening their eyes or upon awakening from sleep — usually months after a history of a corneal abrasion from some mechanical trauma
Corneal Ulcers
- The symptoms of pain, discomfort and photophobia are similar, but patients with ulcers also report redness, watery eyes or mucopurelent discharge as well
- Usually there is a history of contact lens wear or some form of trauma left untreated to develop into a corneal ulcer
Herpes Simplex Keratitis
- The symptoms of pain, discomfort and photophobia are the same; however the etiology of the corneal damage is very different (the case history is very important in differentiating the two)
- Patients with Herpes simplex will not report an initiating insult that caused the corneal damage
Treatment options vary depending on the cause of the corneal abrasion. Patients with contact lens-induced abrasions must have anti-pseudomonas coverage.
Phamacologic Therapy — Cycloplegia
Traumatic iritis may develop one-to-three days after the initial injury. Use cycloplegics only because steroids may delay epithelial healing and increase the risk of corneal infection.
- Atropine 1% for severe abrasions
- Homatropine 5% for moderate abrasions
- Cyclopentolate 1% for mild abrasions
Pharmacologic Therapy — Topical Antibiotic
- Fourth generation fluoroquinolones (Vigamox, Zymar, Ocuflox, Quixin, Besivance) for large abrasions
- Polytrim, Gentamycin, Tobramycin for small abrasions
- Ointments or drops may be used, but ointments offer better barrier function and lubrication between the eyelid and the cornea
Pharmacologic Therapy — Topical NSAID (for pain)
- Acular LS, Nevanac or Prolensa if necessary
Pharmacologic Therapy — Oral Medication
- Oral acetaminophen
- Oral narcotics in severe cases
Surgical Therapy — Amniotic Membrane Placement
Mechanical Therapy — Pressure Patching
- Patching is usually not necessary
- Consider patching if the abrasion is large, if the patient’s discomfort is severe, and/or if the abrasion is healing poorly in the absence of infection
1-day examination
- Assess cornea, determine if patient needs to be patched for a second day
- Consider bandage contact lens
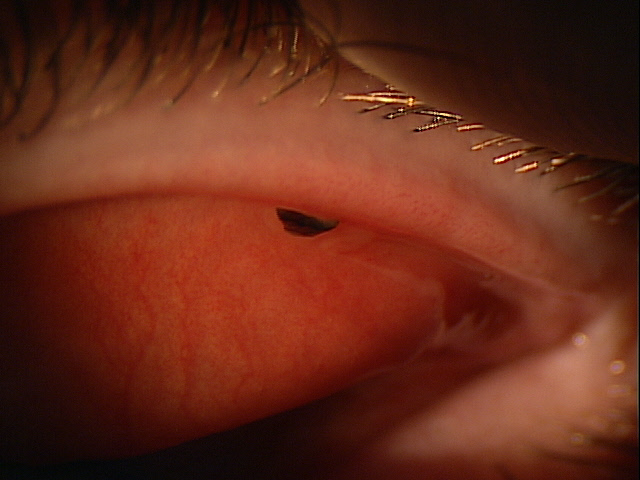
Mechanical Therapy — Bandage Contact Lens
- Low water content bandage contact lens for moderate-to-severe abrasion to relieve pain
- Bed rest, inactivity and OTC analgesics
- Prophylactic topical antibiotics should be used while bandage contact lenses are worn
1-day examination
- Assess cornea, alter topical regimen as appropriate, determine if bandage contact can be removed
- Determine if a hypertonic therapy (sodium chloride 2% or 5% drops/ointment) needs to be added to treat any secondary corneal edema
1. Shah C, Ehlers J. The Wills Eye Manual (fifth edition): Corneal Abrasion. 2008; 15-16.
918.1
Superficial Injury of Cornea
92285
External ocular photography
92071
Bandage contact lens
65778
Amniotic membrane placement
Occurence
- Corneal abrasions are common
Distribution
Corneal abrasions are not distributed evenly throughout the population.
- Younger population affected more
- Physically active individuals affected more
Risk Factors
- Young age
- Physically active




 Print | Share
Print | Share