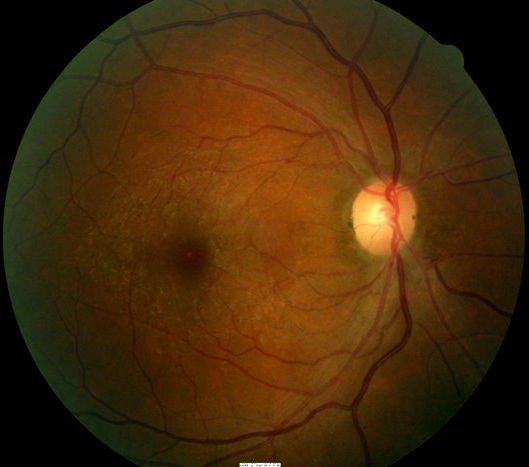
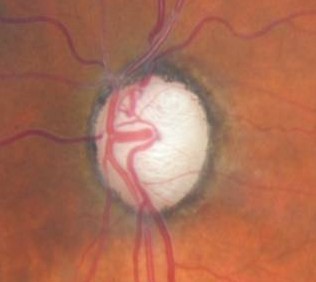
Diffuse pallor of the optic disc in primary optic atrophy
ICD-10 Diagnosis Codes:
H47.211–Primary optic atrophy, right eye
H47.212–Primary optic atrophy, left eye
H47.213–Primary optic atrophy, bilateral
Title
Primary Optic Atrophy
Category
Disorders Of The Optic Nerve And The Visual Pathways
Description
Optic atrophy is the final common morphologic endpoint of any disease process that causes axon degeneration in the retinogeniculate pathway.
- Glaucomatous optic neuropathy
- Hereditary optic neuropathies
- Intracranial trauma
- Compressive lesions in the brain (e.g., tumor or aneurysm)
- Metabolic optic neuropathies (e.g., toxic or nutritional neuropathy, juvenile diabetes)
- Post inflammatory atrophy (e.g., optic neuritis or Devic disease)
- Circulatory optic neuropathies (e.g., central artery occlusion, cranial arteritis, carotid artery occlusion)
The optic nerve is a bundle of nerve fibers that carry images from your retina to your brain. Each fiber carries a part of the visual information to the brain. If these nerve fibers become damaged, the sight may become blurred because the brain isn’t receiving all of this vision information. Optic atrophy means the loss of nerve fibers in the optic nerve.
Structural Damage to the Eye
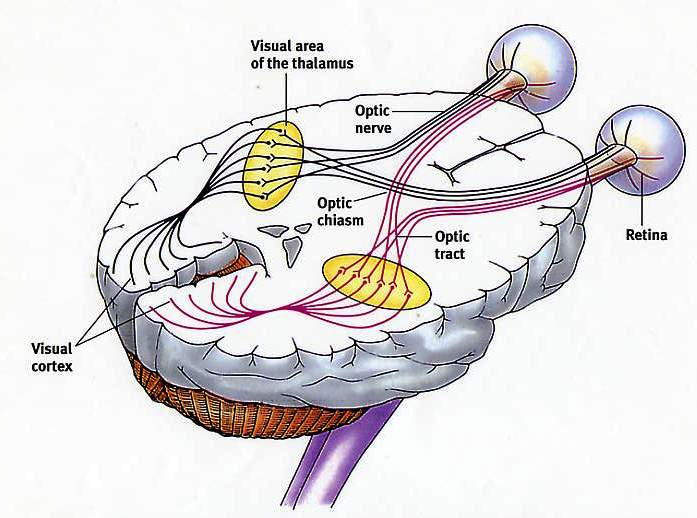 |
Visual Pathway
|
Functional Damage to the Eye
Some of the symptoms that may be associated with optic atrophy include:
- Blurred vision
- Abnormal peripheral vision
- Abnormal color vision
- Decreased brightness in one eye relative to the other
The main goal of the diagnostic evaluation in a patient with optic atrophy is to accomplish the following:
- Make the correct diagnosis of primary vs. secondary optic atrophy (pathologic vs. nonpathologic)
- Determine the underlying cause of the optic atrophy
- Treat the underlying cause if possible
Patient History
Patients will usually present with the following symptoms:
- Painless loss of vision in one or both eyes
Pupillary Examination
- A relative afferent pupillary defect (RAPD) may be present in the affected eye
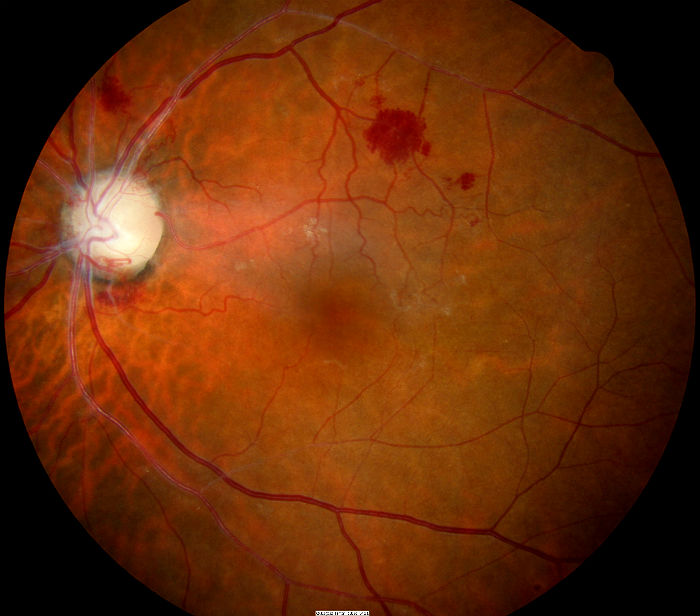
Ophthalmoscopy
- Diffuse pallor of the optic disc in the left eye
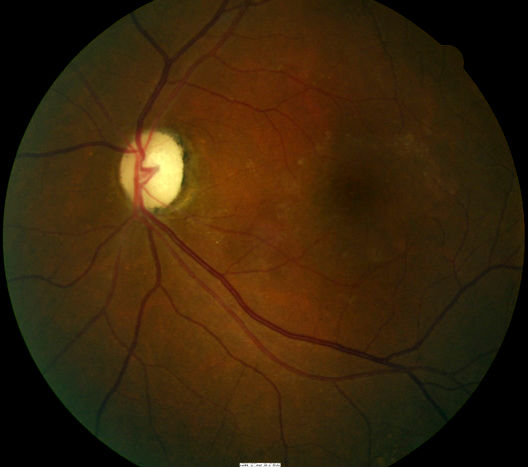
- Thinning/narrowing of the small blood vessels on the optic disc surface in the right eye
DIAGNOSTIC TESTS
The following diagnostic tests can provide clinical information in the evaluation of optic atrophy:
Refraction
- Measuring visual acuity is a method of evaluating functional vision loss
- Primary or secondary optic atrophy, especially in more severe presentations, can produce a loss in visual acuity
- Patient is a 44-year-old black female who experienced a painless loss of vision in the left eye
- Best corrected visual acuity in the right eye = 20/20
- Best corrected visual acuity in the left eye = 20/400
Retinal Scanning Laser
- Can show attenuation of the retinal nerve fiber layer
- Excavation of the optic disc
Visual Field Examination
When a neuro-ophthalmic condition is suspected the most useful testing strategy is the 30-2 threshold visual field. Common findings in patients with optic atrophy include the following:
- Enlargement of the blind spot
- Paracentral scotomas
- Constriction of isopters
- Altitudinal defects
- Bitemporal defects
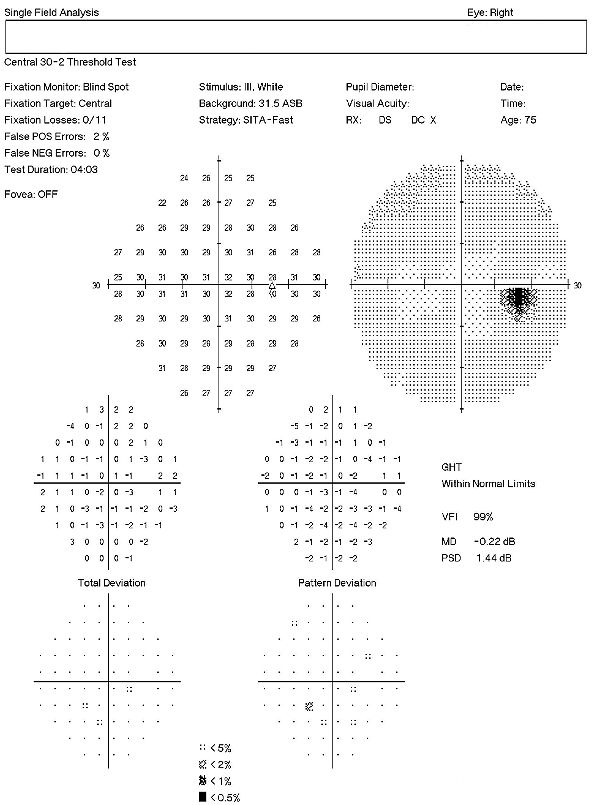 |
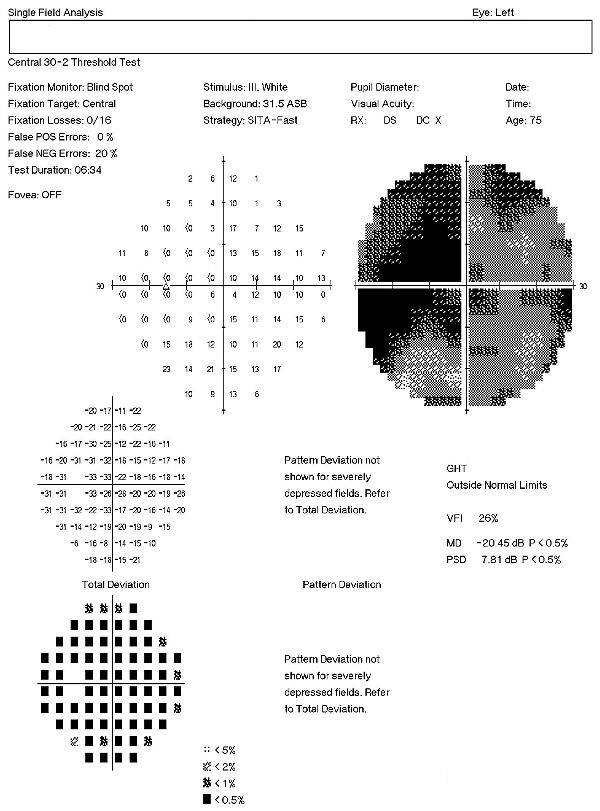 |
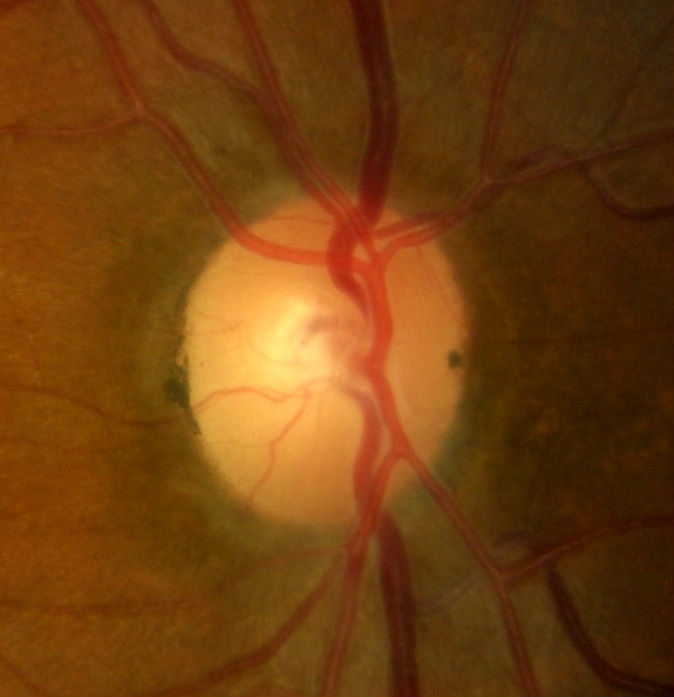
Extended Ophthalmoscopy
- Evaluate optic disc morphology
- Document structural changes to the optic disc
Electrodiagnostics
- Visual evoked potential testing evaluates the function of the afferent visual sensory system
- Pattern electroretinography evaluates the function of the retinal ganglion cells
In optic nerve disease, the amplitude of the visual evoked response is decreased and the latency is delayed compared to the normal eye. In cases of optic atrophy due to compressive lesions, the amplitude of the response is reduced while the latency tends to be normal.
Color Vision Examination
- Measuring color vision is a method of evaluating functional vision loss
- An extended color vision examination measures the combined function of the retina, the optic nerve, and the intracranial visual pathway
- The test is used clinically to detect or monitor color vision loss due to disease at any of these locations
Systemic Evaluation
Eye doctors should consider a systemic evaluation in cases of unexplained optic atrophy. A typical investigative protocol would include the following tests:
- MRI of the brain and orbit with contrast
- Carotid Doppler ultrasound study
- Cardiovascular examination
- Sarcoid examination
- Blood glucose level
- Vitamin B-12 levels
- Antinuclear antibody levels
- Homocysteine levels
- Antiphospholipid antibodies
- Venereal Disease Research Laboratory (VDRL)
Enzyme-linked immunosorbent assay (ELISA)
- Toxoplasmosis
- Rubella
- Cytomegalovirus
- Herpes simplex virus
Primary care eye doctors should communicate as specifically as possible regarding their suspicion of systemic involvement in a patient presenting with primary optic atrophy. This can and should be as detailed as recommending specific laboratory analysis and/or imaging based on the suspected systemic disease.
Optic atrophy is classified as pathologic, ophthalmoscopic, or etiologic.
PATHOLOGIC OPTIC ATROPHY
Anterograde Degeneration
- Deterioration of the retina begins and proceeds toward the lateral geniculate body
- Axon thickness determines the rate of degeneration
- Swelling and degeneration of the axon terminal in the lateral geniculate body is observed as early as 24 hours
Retrograde Degeneration (optic nerve compression by intracranial tumor)
- Deterioration begins from the proximal portion of the axon and proceeds toward the optic disc
- The natural history of this degeneration is independent of the distance of the injury from the ganglion cell body
- Damage to the retrobulbar portion of the optic nerve causes pathologic and visible degeneration of the ganglion cell body simultaneously
Trans-synaptic Degeneration:
- A neuron on one side of a synapse degenerates as a consequence of the loss of a neuron on the other side
- Patients with occipital lobe damage in this type of degeneration have incurred it either in utero or during early infancy
OPHTHALMOSCOPIC OPTIC ATROPHY
Primary optic atrophy
- Optic nerve fibers degenerate in an orderly manner and are replaced by columns of glial cells without alteration in the architecture of the optic nerve head
- Disc is chalky white and sharply demarcated
- Retinal vessels are normal
- Lamina cribrosa is well defined
 |
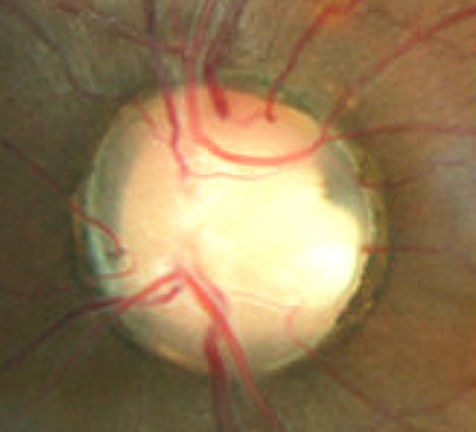
Secondary Optic Atrophy
|
Consecutive Optic Atrophy
- Disc is waxy pale with a normal disc margin
- Marked attenuation of arteries
- Normal physiologic cup
Glaucomatous Optic Atrophy
- Marked cupping of disc
- Vertical enlargement of cup
- Visibility of the laminar pores
- Backward bowing of the lamina cribrosa
- Bayoneting and nasal shifting of retinal vessels
- Splinter hemorrhage at the disc margin may be observed
 |
Glaucomatous Optic Atrophy
|
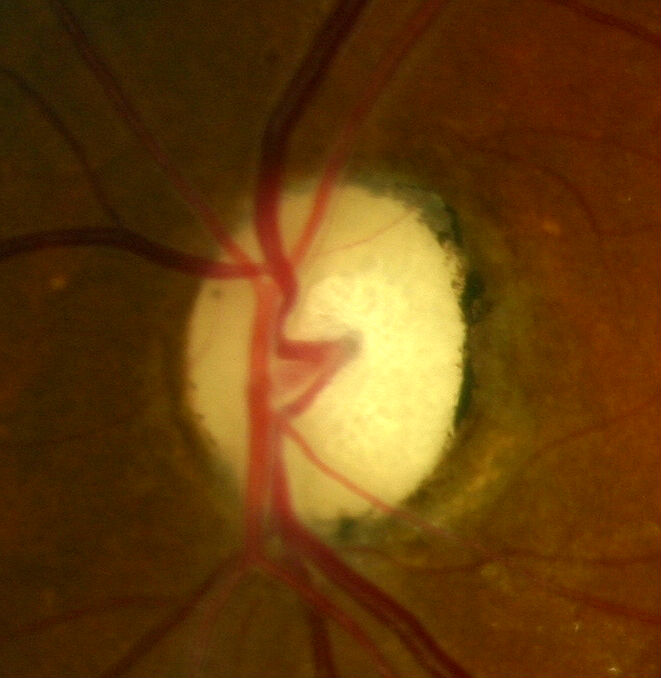
Temporal Optic Disc Pallor
- May be observed in traumatic or nutritional optic neuropathy
- Commonly seen in patients with multiple sclerosis, particularly in those with a history of optic neuritis
- Disc is pale with a clear, demarcated margin and normal vessels
- Physiologic pallor temporally is more distinctly pale
 |
Temporal Optic Disc Pallor — Right Eye
|
ETIOLOGIC OPTIC ATROPHY
Hereditary
- Congenital or infantile optic atrophy (recessive or dominant form)
- Behr hereditary optic atrophy
- Leber optic atrophy
Consecutive Atrophy
- Ascending type of atrophy that usually follows diseases of the choroid or retina
Circulatory Atrophy
- Ischemic optic neuropathy observed when the perfusion pressure of the ciliary body falls below the intraocular pressure
- Observed in central retinal artery occlusion, carotid artery occlusion, and cranial arteritis
Metabolic Atrophy
- Observed in disorders such as nutritional amblyopia, toxic amblyopia, thyroid ophthalmopathy, tobacco, juvenile diabetes, methyl alcohol, and other drugs
Demyelination Atrophy
- Observed in diseases such as multiple sclerosis and Devic disease
Pressure or Traction Atrophy
- Observed in diseases such as glaucoma and papilledema
Post-inflammatory Atrophy
- Observed in diseases such as optic neuritis, perineuritis secondary to inflammation of the meninges, and sinus and orbital cellulites
Traumatic Optic Neuropathy
- Optic nerve avulsion and transection, optic nerve sheath hematoma, and optic nerve impingement from a penetrating foreign body or bony fragment all reflect traumatic forms of optic nerve dysfunction that can lead to optic atrophy
- Traumatic optic neuropathy occurs in 4% of patients with head trauma
- Automobile and bicycle accidents are the most common cause (60% of optic nerve injuries)
There are several conditions that are similar in nature to optic atrophy.
 |
Optic Nerve Pit
|
Myelinated Nerve Fiber Layer
In most patients myelination does not extend past the lamina cribrosa, however, in some patients the nerve fibers are myelinated and manifest as white, feathery patches that follow the nerve fiber layer bundles. The myelinated nerve fibers have a striated appearance and the peripheral edges appear fanned out. The myelination can mimic the appearance of optic disc edema due to elevation of the optic nerve and obscuration of the optic disc margins and vasculature.
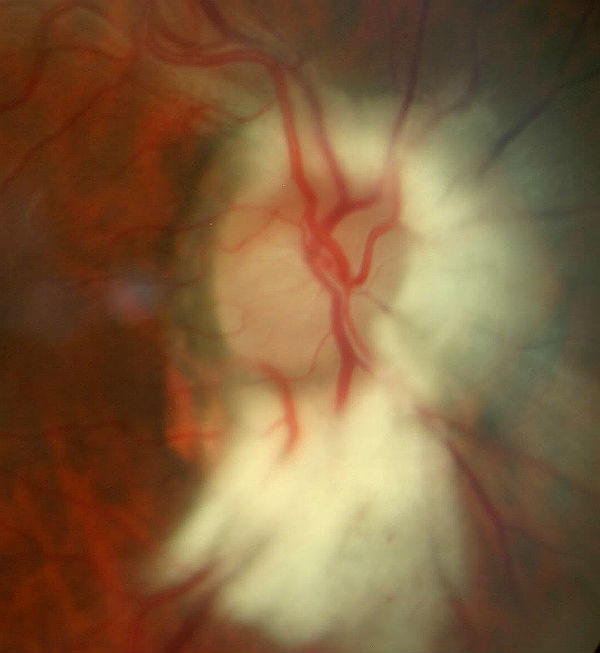 |
Myelinated Nerve Fiber Layer
|
Optic Disc Drusen
Nerve elevation due to disc drusen is usually apparent in childhood as a “full” optic nerve that simulates papilledema. As the person ages and this pseudopapilledema changes, the optic nerve takes on a scalloped appearance at the nasal disc margin. Finally, subtle excrescences appear on the surface of the disc. The drusen enlarge, calcify and become more visible. In later adulthood, the disc elevation decreases, the nerve becomes pale and NFL defects appear.
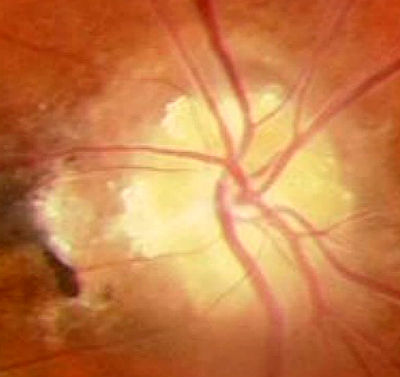 |
Optic Disc Drusen
|
Optic Nerve Hypoplasia
Optic nerve hypoplasia (ONH) is a medical condition arising from the underdevelopment of the optic nerve(s). This condition is the most common congenital optic nerve anomaly. The optic disc appears abnormally small, because not all the optic nerve axons have developed properly. It is often associated with endocrinopathies (hormone deficiencies), developmental delay, and brain malformations. The optic nerve, which is responsible for transmitting visual signals from the retina to the brain, has approximately 1.2 million nerve fibers in the average person. In those diagnosed with ONH, however, there are noticeably fewer nerves.
Scleral Crescent
A myopic crescent is a moon-shaped feature that can develop at the temporal border of disc (it rarely occurs at the nasal border) of myopic eyes. It is primarily caused by atrophic changes that are genetically determined, with a minor contribution from stretching due to elongation of the eyeball. In myopia that is no longer progressing, the crescent may be asymptomatic except for its presence on ocular examination. However, in high-degree myopia, it may extend to the upper and lower borders, or form a complete ring around the optic disc and form a central scotoma.
Tilted Disc
A tilted optic nerve occurs when the nerve exits the eye at an oblique angle. Tilted disc is usually a bilateral condition in which the superiortemporal disc is raised, simulating disc swelling, while the inferiornasal disc is flat or depressed. This results in an oval-shaped disc with the long axis at an oblique angle. The blood vessels also enter the globe at an oblique angle. There is thinning of the RPE and choroid in the inferior nasal quadrant.
Axial Myopia
Myopia, commonly known as near-sightedness, is a condition of the eye where the light that comes in does not directly focus on the retina but in front of it, causing the image that one sees when looking at a distant object to be out of focus, but in focus when looking at a close object. Axial myopia is attributed to an increase in the eye’s axial length.
Brighter-than-normal Luminosity
Presentations in which one eye has a cataract and the other does not usually will give the optic nerve the appearance of being more pale in color in the eye in which no cataract is present.
There is no local (retinal) treatment for primary optic atrophy so no referral to a retinal specialist is warranted. The key to proper treatment is determining the etiology of the optic atrophy because early diagnosis and treatment of the underlying causes of optic atrophy can help prevent further damage from the disease.
For example, early diagnosis and aggressive treatment can prevent further optic nerve damage in patients with compressive and toxic optic neuropathies. In addition, intravenous steroids are helpful in some cases of optic neuritis or anterior ischemic optic neuropathy.
Stem cell treatment can hold a key in the future treatment of neuronal disorders. Neural progenitor cells delivered to the vitreous can integrate into the ganglion cell layer of the retina, turn on neurofilament genes, and migrate into the host optic nerve.
1. Gandhi R. Optic atrophy. Medscape. http://emedicine.medscape.com/article/1217760-overview#a0101. Last accessed April 6, 2014.
2. Optic nerve atrophy. MedlinePlus. http://www.nlm.nih.gov/medlineplus/ency/article/001622.htm. Last accessed April 6, 2014.
3. Optic atrophy. University of Michigan Kellogg Eye Center. http://www.kellogg.umich.edu/patientcare/conditions/optic.atrophy.html. Last accessed April 6, 2014.
4. Optic atrophy. Cleveland Clinic. http://my.clevelandclinic.org/disorders/optic_atrophy/hic_Optic_Atrophy.aspx. Last accessed April 6, 2014.
5. Goodwin D. The differential diagnosis of an optic nerve disorder. RevOptom. 2010 April. http://www.reviewofoptometry.com/continuing_education/tabviewtest/lessonid/106713/. Last accessed Novermber 23, 2014.
377.11
Primary optic atrophy
92015
Refraction
92250
Fundus photography
92083
Visual field examination
92283
Color vision examination
92275
Electroretinography
92225
Extended ophthalmoscopy
92133
Retinal nerve fiber laser scan
92134
Macula OCT scan
95930
Visual evoked potential
Primary Optic Atrophy
Occurrence
The prevalence of visual impairment and blindness attributable to optic atrophy was 0.04% and 0.12%, respectively.
Distribution
Optic atrophy is more prevalent in African Americans (0.3%) than in whites (0.05%).
Risk Factors
- Family history
- Medical history
- Black race




 Print | Share
Print | Share