ICD-10 Diagnosis Codes:
H18.821–Corneal disorder due to contact lens,right eye
H18.822–Corneal disorder due to contact lens,left eye
H18.823–Corneal disorder due to contact lens,bilateral
Title
Corneal Disorder due to Contact Lens
Category
Corneal Opacity And Other Disorders Of Cornea
Description
Contact lens wear can cause a change in corneal physiology, which may lead to lead to epithelial, stromal, and endothelial compromise.
Corneal disorders secondary to contact lens wear vary from mild-to-severe and can occur with any type of contact lens. Corneal disorders may be defined by the corneal layer that is damaged.
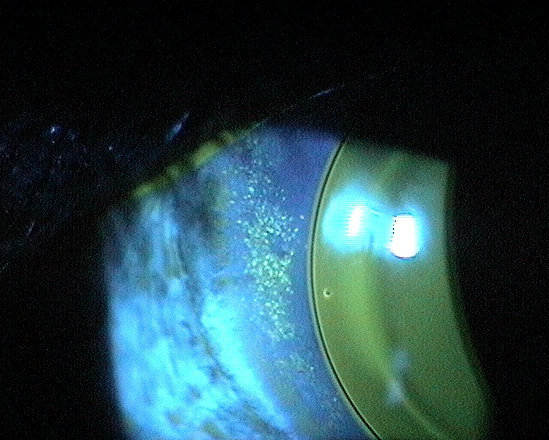
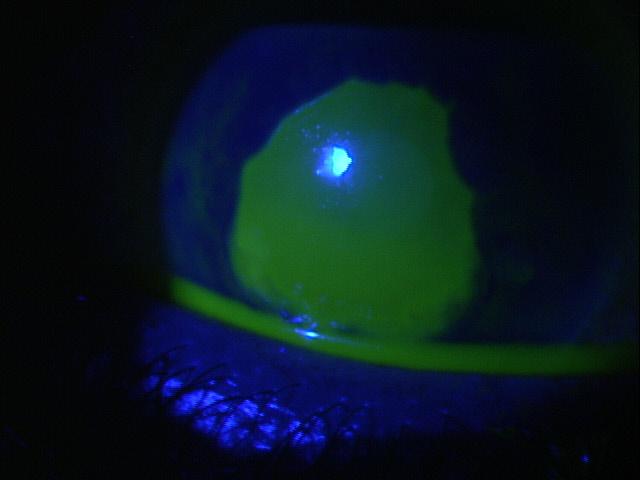
Corneal Epithelium — (anterior cornea)
- Superficial punctate keratopathy
- Epithelial splitting
 |
 |
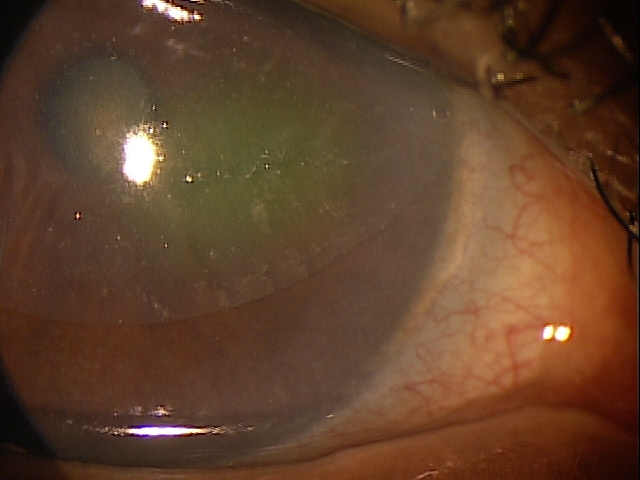
Superficial punctate keratopathy secondary to overnight to contact lens wear
Corneal Stroma — (mid cornea)
- Infiltration
- Loss of transparency
- Neovascularization
Corneal Endothelium — (posterior cornea)
- Increased rate of polymegethism
- Increased guttata formation
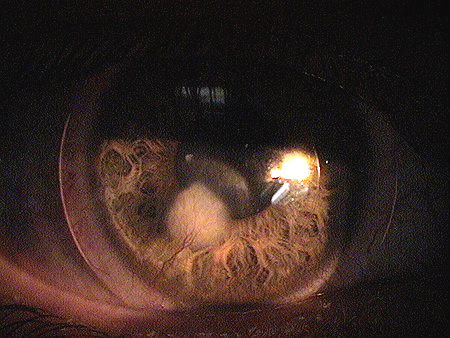
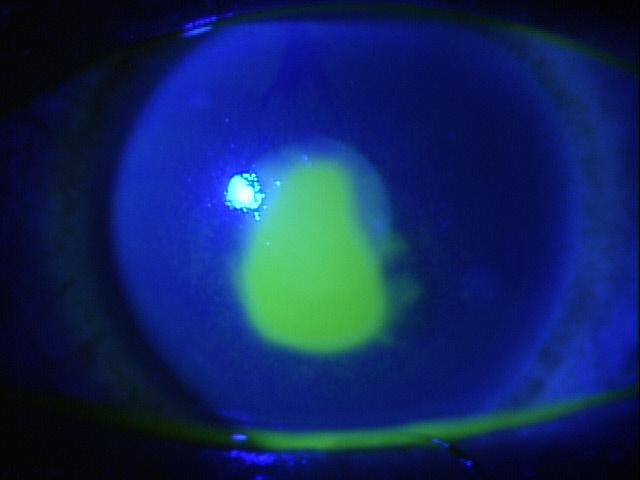
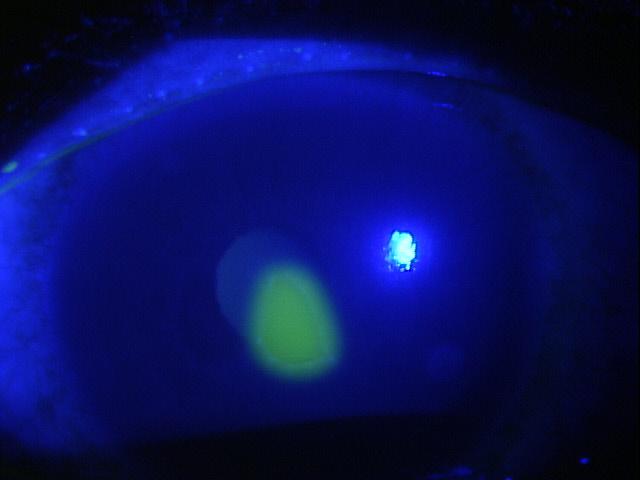
Structural Damage to the Cornea — Epithelial Splitting
Epithelial splits are arcuate-shaped lesions associated with hydrogel and silicone-hydrogel contact lens wear.
There are several explanations for the etiology of epithelial splits:
- One explanation suggests that stiffer contact lenses (e.g., high modulus) have optic zone junction or other back surface changes that through eyelid pressure, exert abnormal force to one spot on the cornea. This mechanically-induced abrasion (epithelial split) may be more common on steeper corneas.
- Another explanation is that the contact lens, due to its design, allows the eyelid to hold debris and stop the tear flow at one area of the cornea. The reduced tear flow leads to poor corneal wetting. In these cases, the debris seen around the lesion may draw inflammatory mediators to the site and initiate an immune response that contributes to the deterioration of the corneal epithelium.
- Last, poor tear film quality and meibomian gland dysfunction may be associated with epithelial splitting.
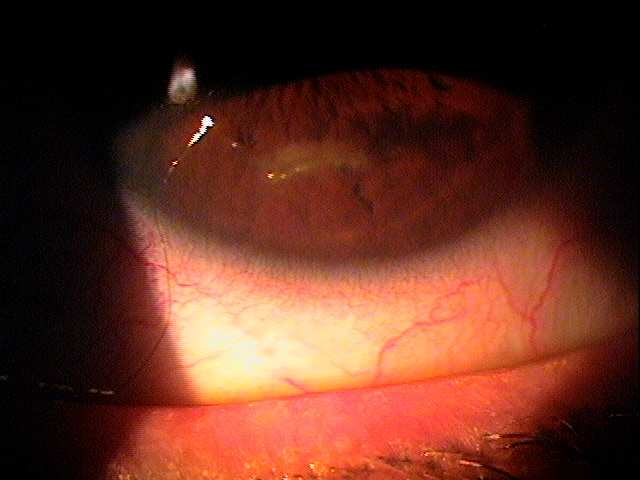 |
Inferior Epithelial Arcuate Lesion
|
|
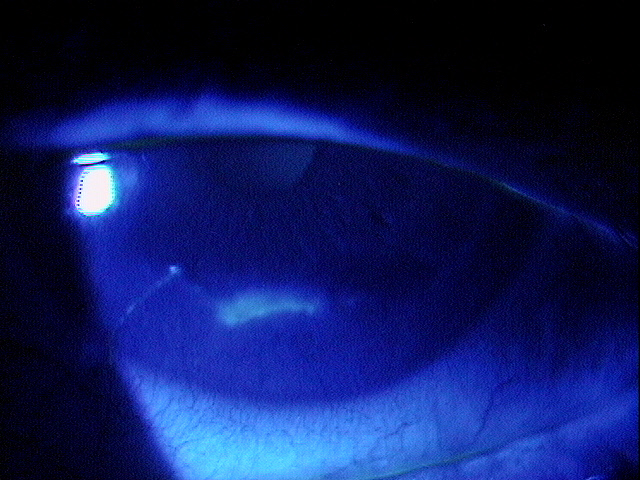 |
Inferior Epithelial Arcuate Lesion
|
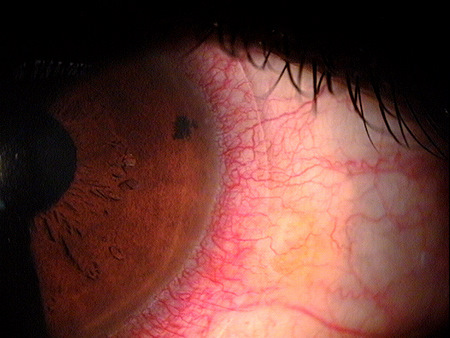
Sturctural Damage to the Corneal Stroma — Neovascularization
Corneal neovascularization is a known complication of wearing contact lenses and both superficial and deep corneal neovascularization are reported with the use of hydrogel, PMMA, and rigid gas-permeable contact lenses.
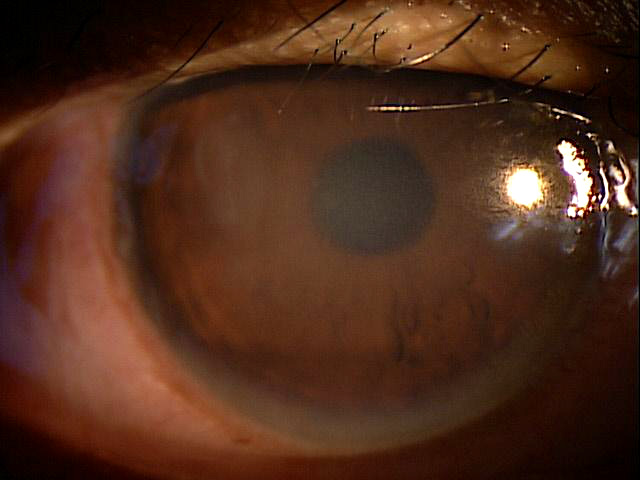
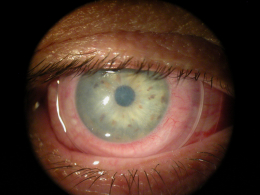
Structural Damage to the Corneal Stroma — Microbial Keratitis (infectious corneal ulcer)
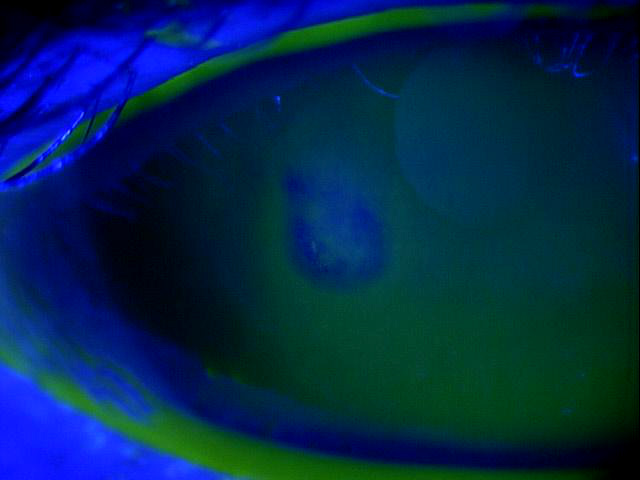
Corneal ulcers usually stain with fluorescein and can be caused by any of the following organisms.
- Bacteria – the most common causes of corneal ulcers and usually caused by gram positive species
- Viral – the most common cause is herpes simplex
- Fungal – needs to be considered if the patient has had traumatic injury with vegetative matter (i.e., tree branches)
- Atypical mycobacteria – ulcers usually seen in patients with major ocular injuries or corneal grafts
- Acanthamoeba – ulcers caused by acanthamoeba are extremely painful and seen in contact lens patients with poor lens hygiene or has a history of swimming with contact lenses on
Bacterial Keratitis
|
 |
 |
Functional Damage to the Eye
- Blurred vision as a result of the compromised cornea
- Corneal edema can result from the insult to the cornea depending on the level of damage
The main goal of the diagnostic evaluation of a patient with a contact lens-induced corneal disorder is to accomplish the following:
- Assess the amount of structural damage to the cornea
- Reduce patients symptoms
- Manage pain accordingly
- Prevent further damage to the cornea
- Reduce re-occurance of damage to the cornea during the healing process
Patient History
Patients with a contact lens-induced corneal disorder may present with any of the following clinical symptoms:
- None
- Acute pain
- Tearing
- Photophobia
- Blurred vision
- Fluctuating vision
- Foreign body sensation
- Blepharospasm
- Pain with eye movements
External Ocular Examination with Biomicroscopy
DIAGNOSTIC TESTS
External Ocular Photography
- Used to document degree of corneal damage
There is no classification system for corneal disorders due to contact lens.
Recurrent Corneal Erosions
- The symptoms of pain, discomfort and photophobia are the same; however the etiology of the corneal damage is very different. The case history is very important in differentiating the two
- Recurrent corneal erosion happen from rubbing their eyes or opening their eyes or upon awakening from sleep – usually months after a history of a corneal abrasion from some mechanical trauma
Corneal Ulcers
- The symptoms of pain, discomfort and photophobia are similar, but patients with ulcers also report redness, watery eyes or mucopurulent discharge as well
- Usually there is a history of contact lens wear or some form of trauma left untreated to develop into a corneal ulcer
The first goal of treating a patient with a corneal disorder due to wearing a contact lens is to discontinue contact lens wear. After that, pharmacologic therapy and/or corneal rehabilitation should be initiated.
Pharmacologic Therapy
Cycloplegia
- Atropine 1% for severe abrasions
- Homatropine 5% for moderate abrasions
- Cyclopentolate 1% for mild abrasions
Topical Antibiotic
- Fourth generation fluoroquinolones (Vigamox, Zymar, Ocuflox, Quixin, Besivance) for severe abrasions
- Polytrim, Gentamycin, Tobramycin for moderate to mild abrasion
Topical NSAID (for pain)
- Voltaran, Acular, Nevanac or Prolenza if necessary
Mechanical Therapy
When treating contact lens-induced corneal abrasions, avoid using bandage contact lenses as a treatment option.
Surgical Treatment
Amniotic Membrane Inserts
1. Suchecki JK, Donshik P, Ehlers WH. Contact lens complications. National Center for Biotechnology Information. 16 Sept 2003. http://www.ncbi.nlm.nih.gov/pubmed/14564768. Last accessed July 22, 2014.
2. Bailey CS. Contact lens complications. Optometry Today. 4 June 1999. http://www.optometry.co.uk/uploads/articles/586d7b2b81d5c23cb892cbef09ce9a6e_Bailey1990604.pdf. Last accessed July 22, 2014.
371.82
Corneal disorder due to contact lens
92285
External ocular photography
65778
Amniotic membrane placement
Occurrence of Epithelial Splitting
- Estimates range from 2%-4% in patients wearing silicone-hydrogel contact lenses on an overnight basis
Distribution
- Corneal abrasions are not distributed evenly throughout the population
- Younger population affected more
- Physically active individuals affected more
Risk Factors
- Youth
- Physically active




 Print | Share
Print | Share