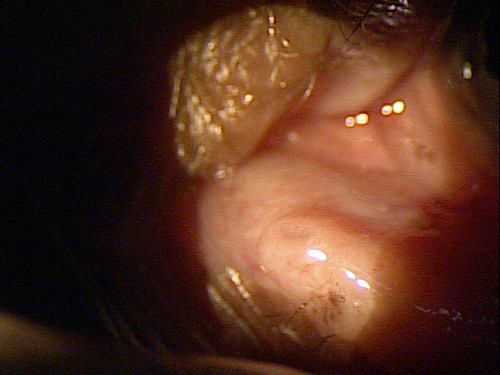
Closed punctal orifice that characterizes punctal stenosis
ICD-10 Diagnosis Codes:
H04.561–Stenosis of right lacrimal punctum
H04.562–Stenosis of left lacrimal punctum
H04.563–Stenosis of bilateral lacrimal punctum
Title
Stenosis of Lacrimal Punctum
Category
Disorders Of The Lacrimal System
Description
A condition characterized by the constriction or narrowing of the lacrimal punctum.
Stenosis of the lacrimal punctum produces a reduction in the tear outflow mechanism and it occurs when there is a constriction, narrowing or obstruction of the punctal orifice. There are two types of acquired stenosis of the lacrimal punctum.
Primary Acquired Nasolacrimal Drainage Obstruction
- A condition that results in inflammatory scarring or fibrosis of the lacrimal punctum
- Unknown etiology
- This type is more common in middle-aged and elderly women
Secondary Acquired Nasolacrimal Drainage Obstruction
- Inflammatory scarring
- Chronic use of medications
- Bacterial, viral or fungal infections
- Surgical injury
- Neoplasm
- Trauma
Strucural Damage to the Eye and Adnexa
- Corneal staining may be involved
- Dry, hyperemic, irritated eyelids from the mechanical wiping
Functional Damage to the Eye
- Distorted, blurred or decreased vision
The main goal of the diagnostic evaluation in a patient with punctal stenosis is to accomplish the following:
- Identify if the stenosis is from a primary or secondary obstruction
- Evaluate any structural obstructions
- Identify and exclude differential diagnoses
- Prescribe a treatment program
Patient History
It is important to differentiate between chronic epiphora, acute epiphora, and normal tearing.
- Chronic epiphora usually results from a persistent or continuous disorder and is more likely to required a dilation procedure
- Acute epiphora usually results from irritative ocular conditions such as corneal foreign bodies, allergic conjunctivitis, dry eye syndrome, eyestrain, or environmental; factors such as wind or cold
- Increases in normal tearing occur during periods of emotional stress or sleep deprivation
External Exam
- Skin around eyelids may appear dry, irritated or red from excessive mechanical wiping
Adnexal Exam
- Eyelids (e.g., ptosis)
- Extraocular muscles
- Orbits
- Preauricular lymph nodes
- Lacrimal apparatus (a network of anatomical structures, appendages, ducts and glands that secrete tears and then drain them from the surface of the eye)
 |
Structures of the Lacrimal Apparatus
|
External Ocular Exam with Biomicroscopy
- Punctal stenosis
- Abnormal tear meniscus height (greater than 2 mm)
- Canaliculitis
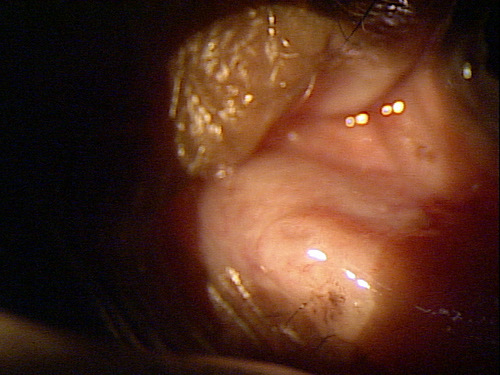 |
Clinical Appearance of the Lacrimal Punctum
|
Clinical Appearance of the Tear Film
|
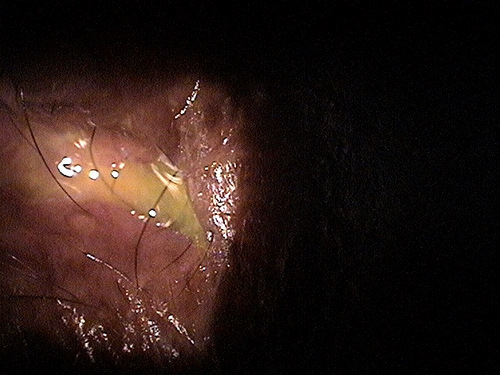 |
Acquired stenosis of the lacrimal punctum are classified into non-specific (idiopathic) and specific acquired obstructions.
Non-specific acquired obstructions are thought to originate from an inflammation of the lacrimal sac. These early inflammatory conditions encourage the mucus membranes in the nasolacrimal canal to release more inflammatory mediators resulting in obstruction of the punctum.
Specific acquired obstructions are caused by inflammatory conditions like sarcoidosis or Wegener’s granulomatosis as well as infections, trauma, surgical injury, foreign bodies, or neoplasm.
Pre-punctal disturbances of ocular surface tear flow
- Ocular allergy
- Dry eye syndrome
- Blepharitis
Non-obstructive causes of epiphora
- Eyelid malposition
Nasolacrimal system obstruction
- The nasolacrimal system may be obstructed rather than the punctum itself
Hordeolum or Chalazion
- These can cause epiphora and make it appear as if there is punctual stenosis
Neurogenic disorder
- Neurogenic disorders or trauma to the seventh cranial nerve can cause hypersecretion
Treatment is aimed at increasing the drainage of the tears and relieving the sypmtoms of epiphora.
- Dilation of the punctum with a lacrimal probe
- Topical anti-inflammatory eyedrops
- Warm compress
|
This video demonstrates the dilation of the punctum |
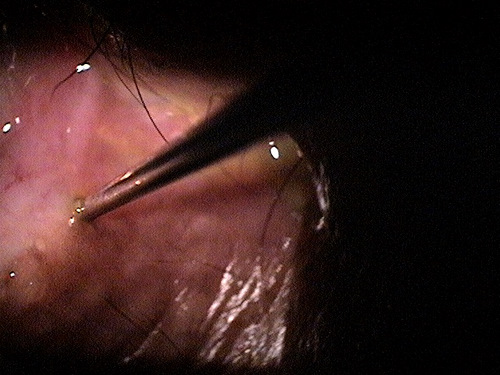
Dilation of the puctum with a lacrimal probe |
1. Soiberman U. Kakizaki H. Selva D. Leibovitch I. Punctal Stenosis: Definition, Diagnosis, and Treatment. National Center for Biotechnology Information. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3402122/. Last accessed August 14, 2014.
2. Tong J. Punctoplasty. Medscape/EMedicine. 28 Feb 2014. http://emedicine.medscape.com/article/1844236-overview#showall. Last accessed August 14, 2014.
3. Morris S. Management of the Chronic Dry Eye Patient. Optometric Management. 1 Apr 2006. http://www.optometricmanagement.com/articleviewer.aspx?articleID=71617. Last accessed August 15, 2014.
4. Legerton J. Schachet J. Look at the Whole Picture. RevOptom. 15 Feb 2007. http://www.revoptom.com/content/d/news_review/c/15509/. Last accessed August 15, 2014.
5. Gilbard J. Dry Eye Natural History, Diagnosis, and Treatment. Ophthalmology Management. 1 Nov 2003. http://www.ophthalmologymanagement.com/articleviewer.aspx?articleid=85952. Last accessed August 15, 2014.
6. Karpecki P. Osmolarity and Dry Eye. RevOptom. 15 Feb 2007. http://www.revoptom.com/content/d/cornea/c/15523/dnnprintmode/true/?skinsrc=%5Bl%5Dskins/ro2009/pageprint&containersrc=%5Bl%5Dcontainers/ro2009/simple. Last accessed August 15, 2014.
7. Karpecki P. Dry Eye: Which Test is Best? RevOptom 15 Feb 2005. http://www.dryeyezone.com/talk/showthread.php?49-Dry-Eye-Which-Test-is-Best. Last accessed August 15, 2014.
375.52
Stenosis of lacrimal punctum
68801
Dilation of the lacrimal punctum
92285
External ocular photography
Occurrence
- Punctal stenosis is common, but the prevalence is unknown
Distribution
- Punctal stenosis is not distributed evenly throughout the population
Risk Factors
- Age-related atrophy of the punctum
- Inflammatory scarring of the punctum
- Trauma to the eyelids
- Female sex
- Chronic use of certain medications




 Print | Share
Print | Share