
Moderate nonproliferative diabetic
retinopathy with macular edema
ICD-10 Diagnosis Codes:
E11.321–Mild nonproliferative diabetic retinopathy, with macular edema
E11.331–Moderate nonproliferative diabetic retinopathy, with macular edema
E11.341–Severe nonproliferative diabetic retinopathy, with macular edema
E11.351–Proliferative diabetic retinopathy, with macular edema
Title
Diabetic Macular Edema
Category
Other Retinal Disorders
Description
A complication of diabetes that occurs when microaneurysms or dilated retinal capillaries leak fluid into the retina.
Diabetes
Diabetes mellitus is a complex, multifactorial and heterogeneous group of disorders characterized by endogenous insulin deficiency and/or insulin resistance. The disease manifests itself as a state of chronic hyperglycemia with attendant microvascular and macrovascular complications.
Diabetic Macular Edema
Macular edema may be present in any stage of diabetic retinopathy and is defined as any one of the following:
- Retinal thickening within 500 microns of the foveal center
- Hard exudates within 500 microns of the foveal center, if associated with the thickening of the adjacent retina
- Retinal thickening greater than one disc area in size, part of which is within one disc diameter of the center of the macul
Structural Damage to the Eye
- Walls of the blood vessels in the retina become fragile and weakened
- Weakened blood vessels have an increase in vascular permeability
- Lipid deposits form in the retinal tissue secondary to chronic edema
- Fluid accumulates in the macula
Functional Damage to the Eye
- Distorted or blurred vision
- Report seeing spots or floaters in field of view
- Report dark or empty spot in the central vision
- Difficulty seeing at night
The main goal of the diagnostic evaluation in a patient with diabetic retinopathy is to accomplish the following:
- Determine the presence or absence of clinically significant macular edema
- If present, classify the severity of the macular edema
- Identify and exclude differential diagnosis
- Prescribe a treatment program
Patient History
The severity of the symptoms or signs is varied and depends on the level of control the patient has over their diabetes. Patients can present with the following abnormal symptoms:
- Blurred vision (sudden or gradual)
- Distorted vision (sudden or gradual)
- Difficulty driving at night
- Floaters or dark spots in their field of view
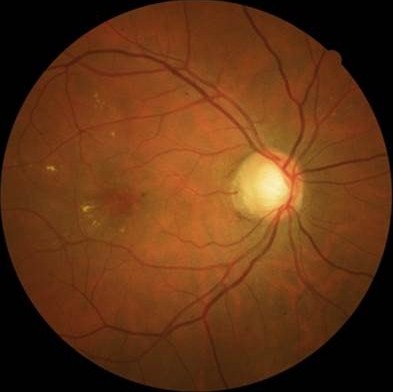
Clinical Appearance of the Retina
The retinal changes associated with diabetic retinopathy include the following:
- Hemorrhages
- Microaneurysms
- Lipid deposits
- Cotton wool spots
- Edema
- Ischemia
- Venous beading
- Intraretinal microvascular abnormalities
- Retinal thickening
- Neovascularization
- Proliferative non-inflammatory degeneration
 |
 |
DIAGNOSTIC TESTS
Refraction
- A method to evaluate the function of the complete visual system
- The function loss of vision secondary to diabetic macular edema is usually determined by the quantification of best corrected visual acuity
- According to The Diabetic Retinopathy Clinical Research Network, a wide range of visual acuity may be observed with varying stages of diabetic macular edema, therefore changes in macular edema have low predictive value compared to visual acuity changes
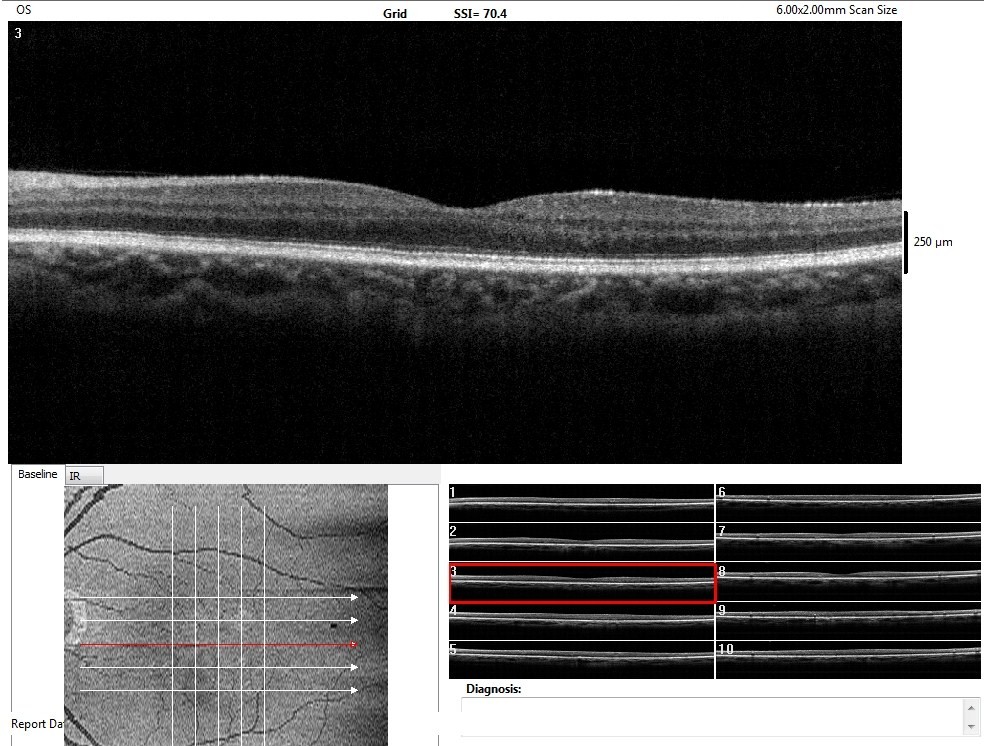
Fundus Photography
Hybrid retinal cameras allow the user to take color photography and one-shot Fundus Autofluorescence Imaging.
- To document the progress or lack of progress of diabetic retinopathy
- To assist in the early diagnosis of diabetic retinopathy
- To assist in staging the disease
- To document the delivery of treatment
- To document the response to treatment
- To help plan a treatment program
 |
 |
|
 |
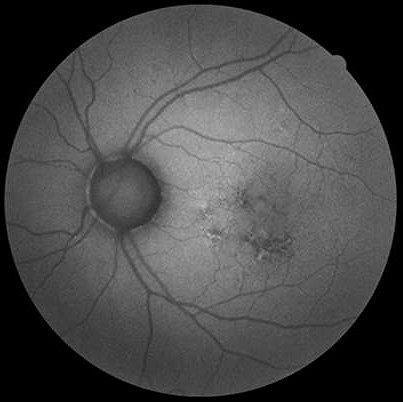 |
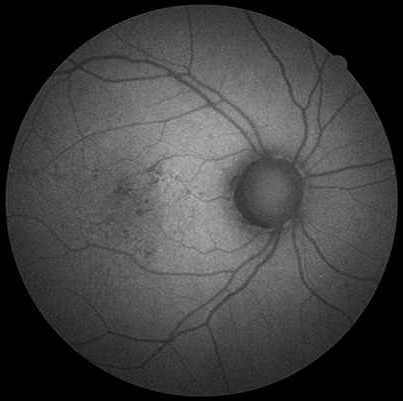
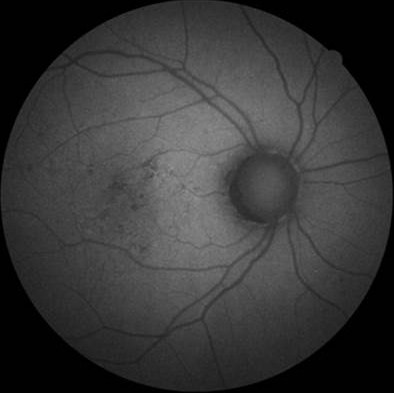
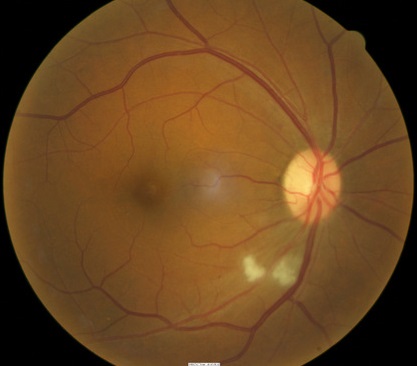
Fundus Autofluorescence (FAF) Imaging
- FAF imaging use infrared light rather than white light for illumination
- FAF imaging evaluates the structure of the retinal pigment epithelium and visualizes the distribution of lipofuscin
- FAF imaging is considered a supplement to color fundus photography
- FAF image may reveal a retinal disorder where the color photograph or OCT does not show abnormality
Abnormal FAF imaging in Both Maculas
- Hyperautofluorescence in the macula of the right eye
- Hyperautofluorescence in the macula of the left eye
Abnormal Color Photography in the Right Macula
- Diabetic macular edema in the right eye (hard exudates at temporal edge of the macula)
- No apparent diabetic macular edema in the left eye
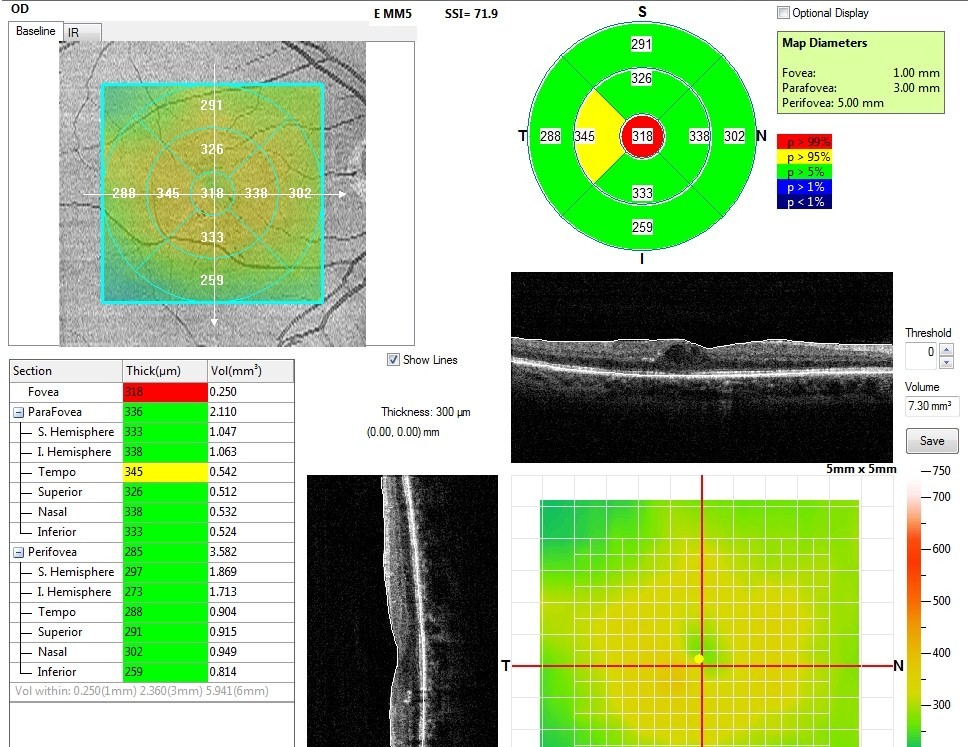
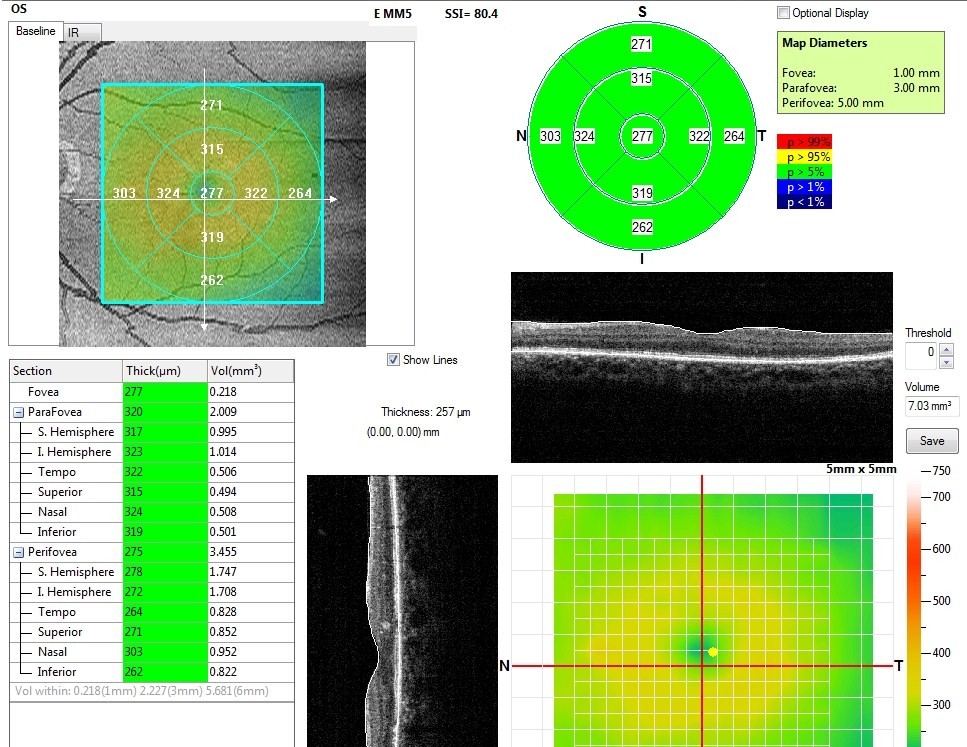
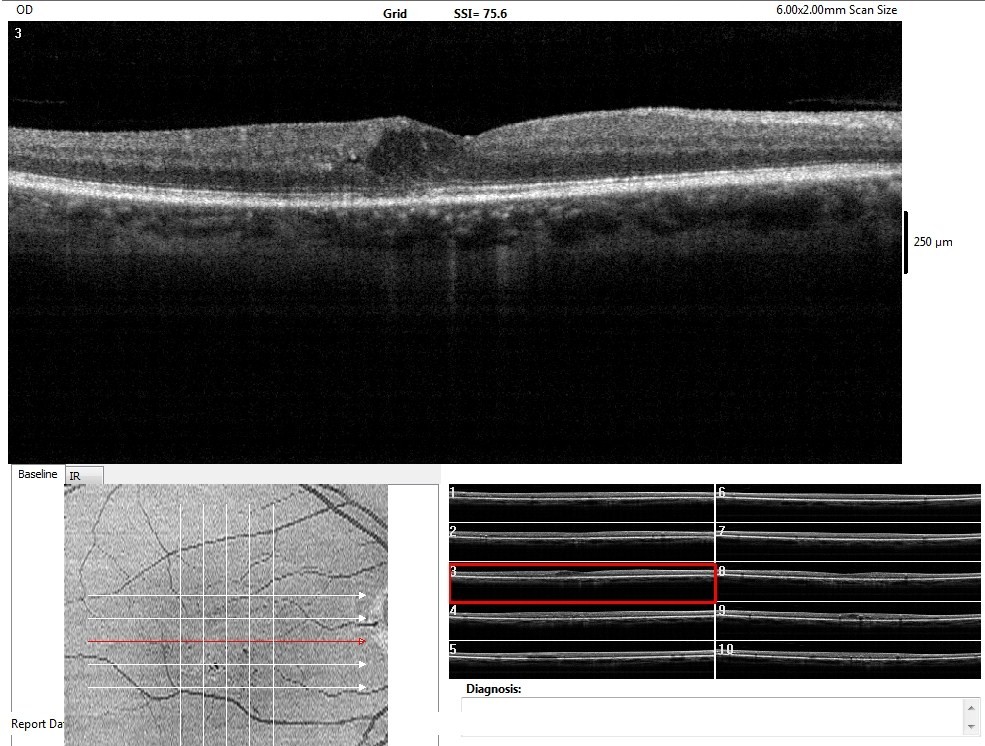
Abnormal OCT Macular Thickness Scan in the Right Macula
- Diabetic macular edema in the right eye (retinal thickening within 500 microns of the foveal center)
- No apparent diabetic macular edema in the left eye
 |
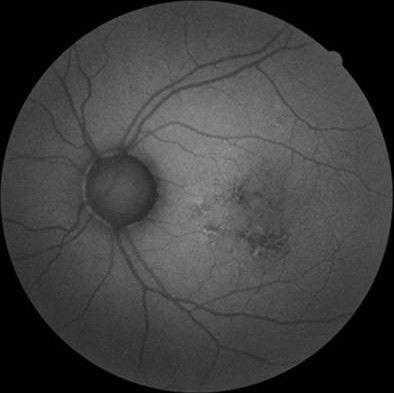 |
Hyperautofluorescence in Diabetic Retinopathy
- Fundus autofluorescence recorded with a Canon CR-2 PLUS Hybrid Digital Retinal Camera
- In patients with diabetes, excess lipofuscin may be an indicator of oxidative damage within the retina
- Macular fundus autofluorescence increases in over 70% of patients with clinically significant diabetic macular edema
- Retinal sensitivity decreases in areas of hyperautofluorescence
- Patterns of hyperautoflourescence (multicystic, single cyst, and combined single- and multicystic)
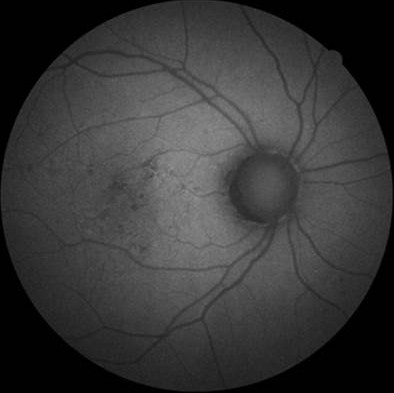 |
FAF Image in Diabetic Retinopathy
|
Retinal Scanning Laser
- To measure the microscopic anatomy of the retina and vitreoretinal interface
- To measure the effectiveness of therapy
- To help in determining the need for ongoing therapy
- To determine the safety of cessation of therapy
 |
 |
|
 |
 |
Visual Field Examination
- Used to assess visual function and determine the size of any associated visual field defects
- Visual field may be affected depending on the size and location of retinal hemorrhaging
the extent of the visual field defect depends on size of macular edema
Diabetic macular edema is classified base on the proximity of retinal thickening or hard exudates to the center of the macula.
 |
No Apparent Diabetic Retinopathy
|
|
 |
Mild Diabetic Macular Edema
|
|
 |
Moderate Diabetic Macular Edema
|
|
 |
Severe Diabetic Macular Edema
|
This would include any eye diseases that produce changes in the retinal vasculature such as hemorrhages, microaneurysms, edema, and exudates.
 |
Hypertensive Retinopathy
|
|
 |
Retinal Venous Obstruction
|
|
 |
Retinal Telangectasia
|
|
 |
Leukemia
|
Most cases of clinically significant macular edema require laser surgery for effective treatment.
Pharmacologic Treatment
- Long term control of blood sugar either through oral medication or injection is important for preservation of vision, especially with no signs of diabetic retinopathy or the early stages of it
Surgical Treatment
 |
Laser Therapy
|
Vitrectomy is a technique in which the vitreous is surgically removed along with the posterior hyaloid. One theory is a vitrectomy may help reduce traction on the macula and this in turn reduces the macular edema. Another theory hypothesis that removing the vitreous removes the cytokines and VEGF associated with a venous occlusive episode. There is no evidence that a vitrectomy is the best treatment.
1. Fabrykowski, MC. Evolving therapies for diabetic macular edema. Rev Optom 2013 Dec 15; 150(12): 52-56.
362.07
Diabetic macular edema
92015
Refraction
92250
Fundus photography
92225
Extended ophthalmoscopy
92134
Macula OCT scan
92083
Visual field examination
92020
Gonioscopy
92275
Electroretinography
92283
Color vision examination
76512
B-Scan ophthalmic ultrasound
Occurrence
- Recent studies reported that 25% of patients with type 2 insulin-dependent diabetes develop diabetic macular edema within ten years of onset
- For type 2 non-insulin dependent diabetes the incidence rate is almost 14%
- Up to 10% of all diabetic patients will eventually develop macular edema
- Diabetic macular edema is seen in up to 3% of patients with mild nonproliferative retinopathy
- Diabetic macular edema is seen in 40% of patients with moderate-to-severe nonproliferative retinopathy
- Diabetic macular edema is seen in 71% of patients with proliferative retinopathy




 Print | Share
Print | Share