ICD-10 Diagnosis Code
B02.39–Other herpes zoster eye disease
Title
Herpes Zoster Dermatitis of Eyelid
Category
Herpes Zoster (1)
Description
Herpes zoster ophthalmicus is a dermalogical and neurologic disorder caused by the varicella-zoster virus.
The herpes zoster virus in its primary form causes varicella or chickenpox. After the primary infection, the virus remains in the dorsal root or other sensory ganglion and may lay dormant for years or decades.
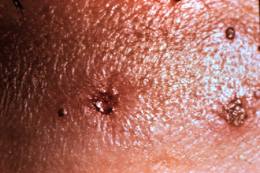
Aging, immunosuppressive illness, new stress, or medical treatment can cause a reactivation of the latent varicelal-zoster virus. Reactivation is characterized by a localized skin rash erupting in a single dermatome called herpes zoster or shingles.
Structural Damage to the Eye and Adnexa
- Vesicular skin rash on the eyelids can lead to scarring
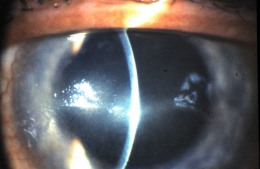
- Corneal scarring can result from infiltrates, stromal edema, or neovascularization
- Corneal ulcers can cause the cornea to become necrotic
- Chronic inflammation secondary to the viral infection can result in structural damage to the cornea
Functional Damage to the Eye
- Profound vision loss due to corneal scarring
- Profound vision loss secondary to corneal necrosis
The main goal of the diagnostic evaluation in a patient with herpes zoster ophthalmicus is to accomplish the following:
- Determine the precise onset of the reactiviation of the virus
- Identify and exclude differential diagnoses
- Prescribe a treatment program
To obtain the information required to determine a clinical diagnosis of herpes zoster ophthalmicus and to prescribe a treatment plan, the following service components of a medical eye examinaion should be performed.
- Patient history
- General medical observation
- External examination
- Adnexal examination
- External ocular examination with biomicroscopy
- Ophthalmoscopy
- Intraocular pressures
Patient History
Patients with herpes zoster ophthalmicus may present with any of the following abnormal clinical signs and symptoms.
- Vesicular skin rash respecting the midline
- Varying degree of pain
- Redness (usually unilateral)
- Foreign body sensation
- Tearing
- Itchy eyes
- Swelling of the eyelids
- Blurred vision
- Fever
- Malaise
External Examination
A face-to-face inspection of the external ocular and facial areas.
Ophthalmoscopy
The ophthalmoscopic examination may reveal some of the clinical signs of herpes zoster opthalmicus – especially in patients that are immunocompromised.
Clinical Appearance of the Retina
- Optic Neuritis
- Optic Papillitis
Clinical Appearance of the Retina
- Posterior pole reaction indicating retinitis
- Posterior pole reaction indicating choroiditis
No specific classification is in place for herpes zoster ophthalmicus.
Herpes simplex virus
The rash associated with herpes simplex does not respect the midline or follow a dermatome. These patients are usually younger. The corneal dendrites of Herpes simplex do have true terminal bulbs and will stain well with fluorescein, while the pseudodendrites of Herpes zoster do not have true terminal bulbs and stains poorly with fluorescein.
Corneal Ulcer
The symptoms of pain, discomfort and photophobia are similar, but patients with ulcers also report redness, watery eyes or mucopurulent discharge as well. Usually there is a history of contact lens wear or some form of trauma left untreated to develop into a corneal ulcer.
Corneal Abrasion
A corneal abrasion at any level can sometimes appear necrotic as well. A corneal abrasion that is healing can be mistaken for a pseudodendritic staining ulcer. Case history is very relevant to differentiate. A preauricular node will not be present for patients with a corneal abrasion.
Cluster Headaches
Sometimes the pain from cluster headaches can mimic skin discomfort and paresthesias. Cluster headaches will not have the accompanying ocular symptoms.
Migraine Headaches
Migraines can also cause pain in and around the eye, skin discomfort and paresthesias. Migraines may or may not be accompanied by visual auras that last about 30 minutes to an hour. Patients other senses may also be heightened or affected during the episode of migraines.
The key to treating herpes zoster ophthalmicus is making an early diagnosis while administering systemic, topical and ophthalmic pharmacologic agents as indicated by the severity of the condition.
Early diagnosis is within 72 hours of viral reactivation (e.g., acute skin rash with active lesions present).
Systemic Pharmacologic Treatment for Skin Involvement
- Acyclovir 800 mg orally 5x / day for 7-10 days; or,
- Famcyclovir 500 mg orally 3x / day for 7-10 days; or,
- Valcyclovir 1000 mg orally 3x / day for 7-10 days
Topical Pharmacologic Treatment for Skin Involvement
- Bacitracin or erythromycin ointment applied to the skin lesions 2x / day for 7-10 days
Supportive Treatment for Skin Involvement
- Warm compress to the periocular skin to keep the area clean 3x / day for 7-10 days
Topical and Systemic Pharmacologic Treatment for Ocular Involvement
- Non-preservative artificial tears can be used in mild forms of herpes zoster ophthalmicus to lubricate the ocular surface
- Prophylactic antibiotic ointment/drops for secondary infections
- Topical steroids to control corneal pseudodendrites, superficial punctate keratitis, neurotrophic keratitis or anterior chamber reactions.
- Topical cycloplegic agent for moderate anterior chamber reactions
- Pain may be severe in the initial two weeks. Analgesics may be recommended. Monitor for post herpetic neuralgia which can have an early onset and last for years.
1. Potter W. An Overview of Ocular Herpetic Disease. May 2010. http://www.reviewofoptometry.com/continuing_education/tabviewtest/lessonid/106745/. Last accessed January 20, 2015.
2. Sowka J. Kabat A. The ‘Other’ Ocular Herpes. RevOptom. 15 July 2009. http://www.revoptom.com/content/d/therapeutic_review/i/786/c/14565/. Last accessed August 17, 2014.
053.20
Other herpes zoster eye disease
92285
External ocular photography
Occurrence
The prevalence of Herpes zoster ophthalmicus is 0-25% of the all herpes zoster cases.
Distribution
- Herpes zoster has a slightly higher prevalence in women than men
- Herpes zoster has a highter prevalence in Caucasians vs. African-Americans
- Herpes zoster ophthalmicus does not seem to correlate with age, gender, or severity of condition
Risk Factors
- Herpes zoster increases dramatically with age
- Herpes zoster increases with immunocompromised individuals




 Print | Share
Print | Share