ICD-10 Diagnosis Code:
B00.52 — Herpes simplex dendritic keratitis
Title
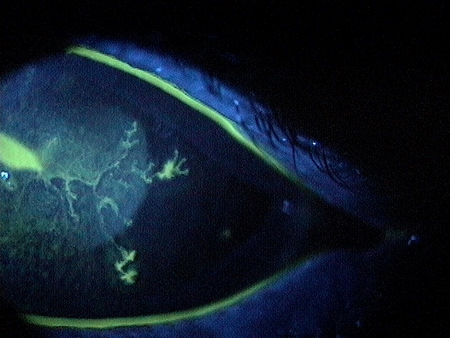
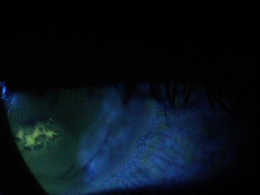
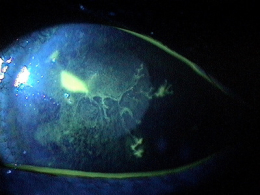
Dendritic Keratitis
Category
Herpes Simplex (1)
Description
Herpes simplex dendritic keratitis is a type of corneal disease caused by the herpes simplex virus (HSV).
Herpetic eye disease is the most common infectious cause of corneal blindness in developed countries.
- The herpes simplex virus (HSV) is responsible for most of these infections
- Up to 500,000 cases of herpes simplex keratitis are reported in the United States each year
Structural Damage to the Eye
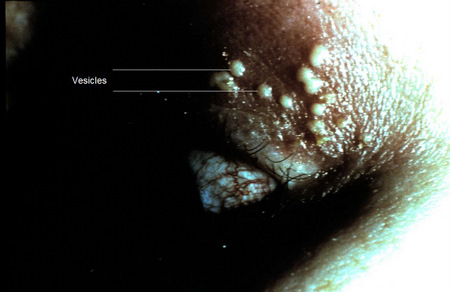
- Vesicular skin rash on the eyelids can lead to scarring
- Ulcers can cause corneal to become necrotic
- Corneal infiltrates, stromal edema and neovascularization can cause scarring
- Inflammatory response in some forms of HSV can result in structural damage
- Damage to corneal nerves can occur in some forms of HSV
Functional Damage to the Eye
- Profound vision loss from scarring and necrosis of cornea
- Loss of corneal sensitivity with some forms of HSV
The goal of the diagnostic evaluation in a patient with dendritic keratitis is to accomplish the following:
- Halt the progression of the disease
- Minimize pain and suffering
- Prescribe a treatment program to manage the corneal infection and prevent permanent vision loss
Patient History
Patients with dendritic keratitis usually present with some or all of the following symptoms:
- Variable degrees of pain
- Ocular redness
- Photophobia
- Foreign body sensation
- Epiphora
Dendritic keratitis may initially present with a vesicular skin rash and follicullar conjunctivitis. The condition is also associated with the following clinical circumstances:
- History of HSV
- Sun exposure
- Fever
- Stress
- Menses
- Trauma
- Illness
- Immunosuppression
External Examination
A face-to-face inspection of the external ocular and facial area.
Adnexal Examination
Look for lymphadenopathy.
- Palpable preauricular lymph node
External Ocular Examination with Biomicroscopy
Evaluate the conjunctiva for a follicular response and the cornea for epithelial damage.
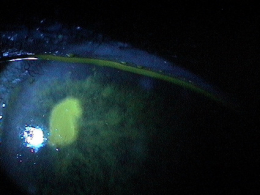
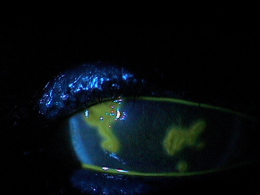
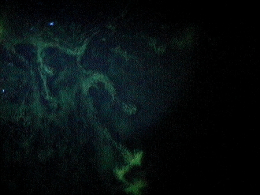
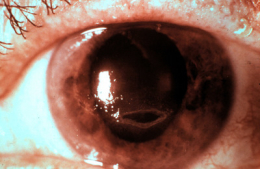
- Small, raised clear vesicles appear on the corneal epithelium and quickly coalesce into a dendritic pattern forming an epithelial defect
DIAGNOSTIC TESTS
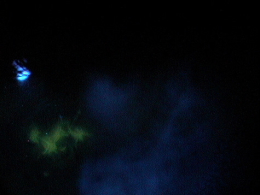
External Ocular Photography
- Document the size, shape, location and extent of the dendritic keratitis
- Document the progression or lack of progression of dendritic keratitis
- Help plan a treatment program
Neurotrophic Keratopathy
This form of HSV is poorly understood. Neurotrophic keratopathy develops in patients with previous HSV epithelial disease. It is neither infectious nor immunologic in origin. Neurotrophic keratopathy arises from impaired corneal innervation and decreased tear formation, exacerbated by long-term use of topical medications like antivirals.
Corneal Stromal Inflammation
This form may be the primary manifestation of HSV keratitis or may be seen secondary to infectious epithelial keratitis, neurotrophic keratopathy, or endotheliitis. The two forms of primary stromal involvement are necrotizing stromal keratitis and ISK.
- Necrotizing stromal keratitis is caused by a direct infection of the corneal stroma and result is a severe inflammatory response. Necrotizing stromal keratitis is characterized by dense stromal infiltrate, ulceration, and necrosis. It is a result of viral replication in stromal keratocytes and the inflammatory response. This intrastromal inflammation can lead to thinning and perforation within a short period. The use of topical corticosteroids without antiviral coverage may be a possible risk factor for its development.
- ISK is an antibody-complement cascade triggered by retained viral antigen within the stroma. ISK is a common manifestation of chronic recurrent ocular HSV disease. ISK may present clinically with focal, multifocal, or diffuse cellular infiltrates; immune rings; neovascularization; or ghost vessels at any level of the cornea.
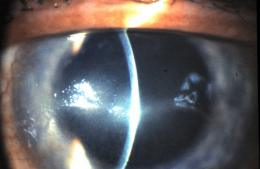
Endotheliitis
This form is an immunologic reaction to an antigen in endothelial cells and a suspected cause from the live virus as well.
- Clinical signs of endotheliitis are keratic precipitates, overlying stromal and epithelial edema and an absence of stroma infiltrate or neovascularization. A mild-to-moderate iritis is seen.
- HSV endotheliitis can be further classified as disciform, diffuse, or linear.
- Disciform endotheliitis appear as round patches of central or paracentral corneal edema with a clear demarcation between involved and uninvolved cornea.
- Diffuse endotheliitis presents with scattered keratic precipitates and may stem from a previous disciform area of involvement.
- Linear endotheliitis shows a line of keratic precipitates progressing centrally from the limbus. There may be peripheral corneal edema trailing the migrating line of keratic precipitates. The line of keratic precipitates can be sectoral, circumferential, straight or serpiginous pattern.
Corneal Abrasion
- A corneal abrasion at any level can sometimes appear necrotic as well
- A corneal abrasion that is healing can be mistaken for a dendritic staining ulcer
- Case history is very relevant to the differential diagnostic process
- A preauricular node will not be present for patients with a corneal abrasion
Recurrent Corneal Erosion
- Case history is important in differentiating recurrent corneal erosion versus the punctate epithelial erosions found in neurotrophic keratopathy
- Patients with RCE will usually wake up with symptoms in the morning, upon wakening or after having eyes shut for a period of time
- A preauricular node will not be present for patients with recurrent corneal erosion
Herpes Zoster
- These patients will also experience the painful skin vesicles that do not cross the midline
- The herpes zoster patient can sometimes experience the pain before the vesicles appear
- The pseudodendrites in herpes zoster are raised mucous plaques and do not have terminal end bulbs like in HSV
- These plaques also do not stain well with fluorescein in comparison to the dendritic ulcers of HSV
Bacterial Keratitis
- The distinctive symptom is a copious mucopurulent discharge
- Patient symptoms can vary depending on how long the eye has been infected
- Patients will often report being ill with some form of sinus or nasal related bacterial infection
Fungal Keratitis
- A fungal ulcer shpuld be considered if a patient has had traumatic injury with vegatative matter (e.g., tree branch)
- Fungal infiltrates have feathery borders surrounded by satellite lesions
- Culture can confirm the diagnosis if everything else is ruled out
Interstitial Keratitis
- Patients with interstitial keratitis will have the same symptoms as HSV
- This should be considered but usually can be ruled out from the case history
- Acute interstitial keratitis occurs in the first or second decade of life and then old signs of it persist through life since the common etiology is congenital syphilis
- Less common etiologies is from acquired syphilis, tuberculosis, Cogan’s syndrome, Lyme disease and Herpes simplex virus, so it has to be considered as a differential diagnosis
- The critical sign for interstitial keratitis is the patient will have corneal stromal blood vessels and edema
- Signs of a reoccurring disease will show deep corneal haze or scarring, corneal stromal blood vessels with minimal or no blood and corneal stromal thinning can be seen
Acanthamoeba Keratitis
- Acanthamoeba related ulcers are extremely painful even though the overall eye looks relatively quiet
- A case history usually reveals a patient with poor contact lens hygiene or a history of swimming with contact lenses
- A culture can confirm the diagnosis if everything else has been ruled out
Sicca Keratoconjunctivitis
- Symptoms are also very similar, but patients with dry eye from aqueous deficiency will have a reduced tear film volume
- In patients with evaporative dry eye syndrome, an insufficient lipid layer secondary to meibomian gland disease will produce frothing along the eyelid margin and an abnormal tear film break-up time
Corneal Ulcer
- The symptoms of pain, discomfort and photophobia are similar, but patients with ulcers also report redness, watery eyes or mucopurulent discharge as well
- Usually there is a history of contact lens wear or some form of trauma left untreated to develop into a corneal ulcer
The primary goals of treating acute herpetic keratitis include the following:
- Stop viral replication
- Prevent permanent vision loss
Current best practices includes the use of Zirgan (ganciclovir ophthalmic gel 0.15%) from Bausch & Lomb.
Pharmacologic Treatment: Topical Antiviral Medications
Zirgan Ophthalmic Gel
- Recommended dosing regimen is one drop in the affected eye five times daily until the ulcer heals
- After the ulcer heals, continue treatment with one drop three times per day for seven days
Viroptic Ophthalmic Solution
- Gentle debridement of the ulcer bed to remove active virus cells
- Topical trifluridine 1% solution 1 gtt q2h not to exceed 8gtt/day for approximately 7-10 days
- As the dendrites begin to regress, taper the dosage to q3-4h until the lesion resolves completely
- Complete resolution of the dendritic lesions usually occurs in 7-10 days
- Topical acyclovir ointment applied to lower conjunctival sac 5 times/day at 4 hour intervals for 10 days
- Response to topical therapy usually occurs in 2-5 days, with complete resolution in 2 weeks
Corneal toxicity is a frequent adverse effect of topical antiviral agents. Therefore, topical therapy should be tapered rapidly after initial response and discontinued after complete healing, generally within 10-14 days. Failure of epithelial healing after 2-3 weeks of antiviral therapy suggests epithelial toxicity, neurotrophic keratopathy, or, rarely, drug-resistant strains of HSV.
Topical Cycloplegic Agents
- May be needed if there is a secondary anterior uveitis
- Homatropine 2% or 5% (t.i.d. – q.i.d.)
- Scopolamine 0.25% (b.i.d. – q.i.d.)
Topical Steroids
- Topical steroids are contraindicated in active infectious epithelial HSV keratitis
Pharmacologic Treatment: Oral Medications
- Oral acyclovir (2g/d) has been reported to be as effective as topical antivirals for acute herpetic keratitis
- Oral medications are preferred over topical agents for patients with preexisting ocular surface disease who are at high risk for toxicity from topical medications, immunocompromised patients and pediatric patients
Mechanical Treatment for Neurotrophic Keratopathy
- Non-preserved lubricants
- Eyelid patching
- Bandage contact lenses
- Potentially epithelial toxic medications should be discontinued
- Surgical intervention such as tarsorrhaphy may be required if the patient does not respond to any of the above regimen
Corneal Stromal Inflammation and Endothelitis
- Combination treatment with topical conticosteroids and antiviral
- Initially frequent topical steroids prescribed and the dosage is titrated to the lowest dosage necessary to control the inflammation based upon clinical response
- Concurrent topical antiviral is utilized to prevent epithelial keratitis
- Optimal combination dosage has not been determined
- One recommendation from literature is to use a topical antiviral and a topical corticosteroid with equal frequency until the steroid can be reduced to once a day or less
- Alternatively oral acyclovir (1-2 g/day) can help achieve the same therapeutic concentration in the aqueous and may be more effective in treating uveititis and keratitis from HSV
- In the necrotizing stromal keratitis, a systemic antiviral may be a better alternative since corneal toxicity is a concern
1. Potter WB. An overview of ocular herpetic disease. Rev Optom 2010 May 15; 157(5):76-81. http://www.revoptom.com/continuing_education/tabviewtest/lessonid/106745/. Last accessed August 12, 2014.
2. Silbert J. Is It An Ulcer Or an Infiltrate? RevOptom. 15 June 2007. http://www.revoptom.com/content/d/cornea/c/15408. Last accessed August 12, 2014.
3. Lasswell L. Huth S. Tran. Much Ado About Staining. Rev Optom. 15 Nov 2006. http://www.revoptom.com/content/d/news_review/c/17001/dnnprintmode/true/?skinsrc=%5Bl%5Dskins/ro2009/pageprint&containersrc=%5Bl%5Dcontainers/ro2009/simple. Last accessed August 12, 2014.
4. Edwards K. Brian G. Stretton S. Stapleton F. Willcox M. Sankaridurg P. Sweeney D. Holden B. Microbial Keratitis and Silicone Hydrogel Lenses. Contact Lens Spectrum. Jan 2004. http://www.clspectrum.com/articleviewer.aspx?articleid=12494. Last accessed August 12, 2014.
Dendritic keratitis
92015
Refraction
92285
External ocular photography
Occurrence
- Annually, there are 20,000 new cases of ocular HSV in the United States and more than 28,000 reactivations per year
- HSV keratitis is the most frequent cause of corneal/infectious blindness in the United States
- HSV keratitis is also the most common cause of infectious blindness in the Western world
Distribution
- Herpes simplex dendritic keratitis is distributed evenly throughout the population
Risk Factors
- Advanced age
- Occurs in adults more than in children




 Print | Share
Print | Share