Abnormal tear meniscus height secondary
to nasolacrimal ductobstruction
ICD-10 Diagnosis Codes:
H04.551–Acquired stenosis of right nasolacrimal duct
H04.552–Acquired stenosis of left nasolacrimal duct
H04.553–Acquired stenosis of bilateral nasolacrimal ducts
Title
Acquired Stenosis Of Nasolacrimal Duct
Category
Disorders Of The Lacrimal System
Description
The nasolacrimal duct is a channel that allows tears to drain from the external eye to the nasal cavity. A nasolacrimal duct obstruction is an acquired or congenital obstruction of the drainage system resulting in epiphora or excessive tearing.
Corneal edema is a clinical sign of corneal disease. The condition is characterized by an increase in corneal thickness secondary to an abnormal accumulation of fluid. The excess fluid produces a swelling of the corneal tisssue and can result in a loss of stromal transparency that produces blurred vision or visual impairment.
A congenital nasolacrimal duct obstruction results from a membrane in the duct that did not spontaneously perforate as expected at birth. Acquired nasolacrimal duct obstructions can be non-specific (idiopathic) or specific in nature. Non-specific obstructions are thought to originate from an inflammation of the lacrimal sac, while specific obstructions are linked to inflammatory diseases.
Other causes of acquired specific obstructions include the following:
- Infection
- Trauma
- Surgical injury
- Neoplasm
Structural Damage to the Eye
- If an infection is present, a palpable mass may appear at the inner canthus
- Palpebral conjunctiva may have papillae as a result of the body’s response Staphylococcus aureus
- Physical examination of eyelids can show signs of edema, hyperemia and tender to touch
- Extent of signs and symptoms found depends on the cause of obstruction
Functional Damage to the Eye
- Distorted, decreased or obstructed vision secondary to excessive tears or excessive blinking
The main goal of the diagnostic evaluation in a patient with nasolacrimal obstruction is to accomplish the following:
- Determine the etiology of the obstruction and determine whether it is congenital or acquired
- Alleviate the symptoms
- Determine a treatment program
Patient History
Patients with nasolacrimal obstruction will present with the following abnormal clinical signs and symptoms:
- Excessive tearing
- Pain around the inner corners of the eye
- Discharge around the inner corners of the eye
External Ocular Examination with Biomicroscopy
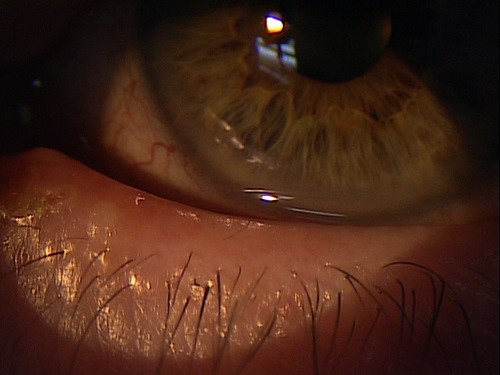 |
Clinical Appearance of the Eyelid
|
|
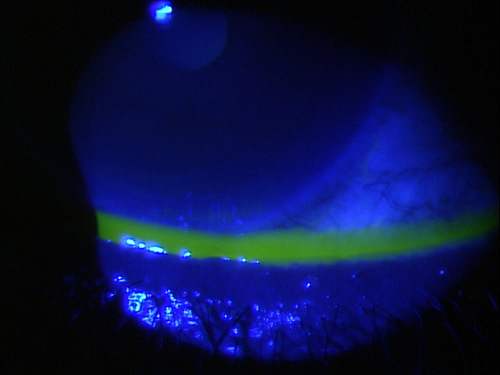
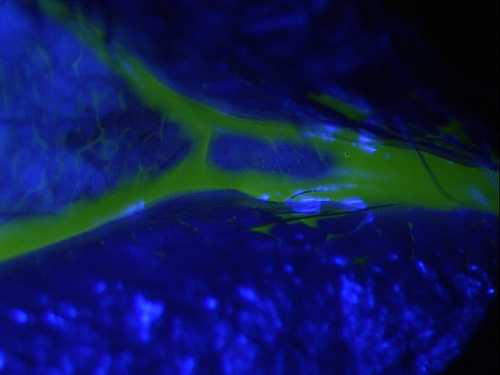
Clinical Appearance of theTear Film
|
 |
DIAGNOSTIC TESTS
External Ocular Photography
- To document the progress or lack of progress of a condition
Congenital Obstruction
- Congenital nasolacrimal obstructions are a result of an imperforated membrane that usually spontaneously opens at the time of birth. Sometimes the membrane can persist and extend into adulthood. By the first year of age, if the membrane has not spontaneously perforated, then the probing of the membrane is a successful treatment option. After the age of six, the success rate of probing declines significantaly and a surgical treatment called dacryocystorhinostomy (DCR) is preferred.
Acquired Obstruction
- Acquired Obstructions are often classified into non-specific (idiopathic) and specific acquired obstructions.
- Non-specific acquired obstructions are thought to originate from an inflammation of the lacrimal sac. These early inflammatory conditions encourage the nose and the respiratory-like mucus membranes in the nasolacrimal canal to release more inflammatory mediators resulting in obstruction of the structure.
- Specific causes of nasolacrimal obstructions are caused by inflammatory conditions like sarcoidosis and Wegener’s granulomatosis as well as infections, trauma, surgical injury, foreign bodies, or neoplasm of the lacrimal sac and duct.
- Dacryocystitis is an infection of the lacrimal sac and can be classified as acute, subacute or chronic. It may be localized or extend to other orbital tissue and lead to pericystitis or orbital cellulites. If it is localized to the lacrimal sac, a palpable mass can be found at the inner canthus of the involved eye. As the infection develops, the nasolacrimal sac pushes on the canaliculus and prevents the sac from being reducible. As a result, the chronic stasis and build up of material leads to an infection. Staphylococcus aureus is the common bacteria causing the infection
Punctal Stenosis
- The punctum has become blocked by some means, while the lacrimal canaliculi and nasolacrimal duct are patent
Patients with epiphora of unknown etiology should undergo a thorough lacrimal evaluation that includes at least the following:
- Consideration by history and physical examination (including slit lamp), of likely pre-punctal and/or non-obstructive causes for epiphora such as disturbances of ocular surface tear flow by eyelid malposition, allergy, dry eye, and blepharitis
- Non-invasive testing to diagnose punctal or post-punctal obstruction and to identify the site and degree of obstruction, such as by using dye disappearance testing when appropriate
- Initiation of appropriate treatment
Dilation of the Lacrimal Punctum without Irrigation
|
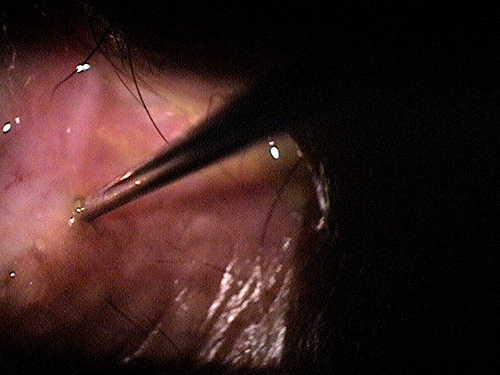 |
|
 |
Dilation of the Lacrimal Punctum with Irrigation
|
|
Nasolacrimal Obstruction
|
 |
Intraocular Surgery
- Dacryocystorhinostomy (DCR) is a surgical procedure where the lacrimal sac is drained into the nose
1. Camara J. Obstruction Nasolacrimal Duct. Medscape/EMedicine. http://emedicine.medscape.com/article/1210141-overview#showall. Last accessed August 13, 2014.
2. Dacryostenosis. The Merck Manual. Oct 2013. http://www.merckmanuals.com/professional/eye_disorders/eyelid_and_lacrimal_disorders/dacryostenosis.html. Last accessed August 13, 2014.
375.56
Acquired stenosis of nasolacrimal duct
68801
Dilation of the lacrimal punctum
68840
Probing of the nasolacrimal canniliculus
68810
Probing of the nasolacrimal duct
92285
External ocular photography
Occurrence
- Nasolacrimal obstruction is relatively common but the prevalence is unknown
Distribution
- Nasolacrimal obstruction is not distributed evenly throughout the population
Risk Factors
- Female sex
- Age
- Past trauma to area
- Hormonal changes in females




 Print | Share
Print | Share