Visual field defect cause by location
ICD-10 Diagnosis Codes:
H53.411–Central scotoma, right eye
H53.412–Central scotoma, left eye
H53.413–Central scotoma, bilateral
H53.421–Enlarged blind spot, right eye
H53.422–Enlarged blind spot, left eye
H53.423–Enlarged blind spot, bilateral
H53.431–Sector or arcuate defects, right eye
H53.432–Sector or arcuate defects, left eye
H53.433–Sector or arcuate defects, bilateral
H53.531–Other localized visual field defect, right eye
H53.532–Other localized visual field defect, left eye
H53.533–Other localized visual field defect, bilateral
H53.461–Homonymous bilateral defects, right side
H53.462–Homonymous bilateral defects, left side
H53.47–Heteronymous bilateral field defect
H53.481–Generalized contraction, right eye
H53.482–Generalized contraction, left eye
H53.483–Generalized contraction, bilateral
Title
Visual Field Defect
Category
Visual Disturbances
Description
Visual defects are localized defect in a person’s visual field. They can occur from a variety of causes such as trauma to the brain or visual pathway, diseases and disorders of the eye, optic nerve or the brain and systemic vascular disease
Visual defects are localized defects in a person’s visual field. They can occur from a variety of causes such as trauma to the brain or visual pathway, diseases and disorders of the eye, optic nerve or the brain and systemic vascular disease.
Structural Damage to the Eye
- Damage of retinal ganglion cells
- Damage of visual cortex or neurological visual pathways
Functional Damage to the Eye
- Associated visual field defects
The main goal of the diagnostic evaluation for a patient with visual field defect is to accomplish the following:
- Determine the etiology of the visual defect
- Determine the structural and/or functional damage to the eye
- Develop a treatment plan
Patient History
Patients with visual field defects will have the following abnormal clinical signs and symptoms:
- Visual distrubances
- Isolated regions of vision loss
- Overall loss of vision, blur, discomfort of vision
Additional factors to determine in the patient history:
- Is the vision loss sudden or gradual
- Does he visual field defect appear to be a spot, a region of blur or does the overall view of objects has missing parts
- Did the patient have any recent history of trauma
- Does the patient have a history of eye diseases such as glaucoma, optic nerve disorder, neurological disorder or vascular disease
- Did the patient have a recent stroke or heart attack
Clinical Appearance of the Retina
|
 |
DIAGNOSTIC TESTS
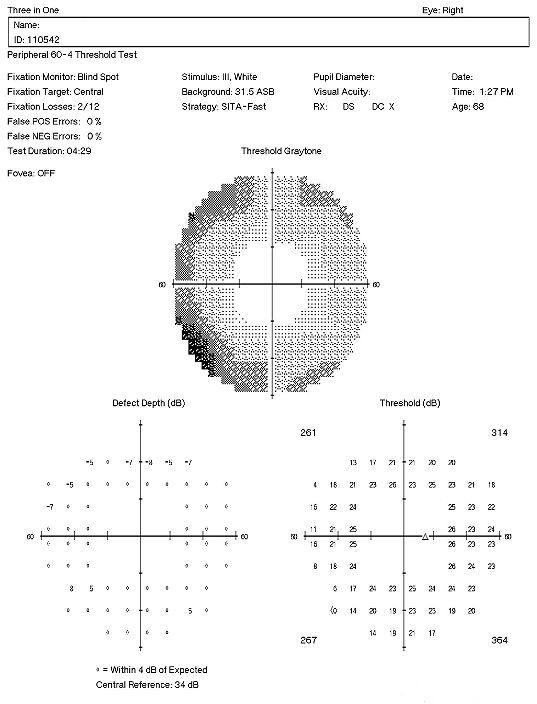
The main goal of the diagnostic testing is to accomplish the following:
- Confirm the etiology of the visual field defect
- Determine the extent of the visual field defect
- Determine the structural and functional damage to the eye
- Evaluate progression or improvement of visual field defect over time
Refraction
- Measurement of visual function / visual acuity
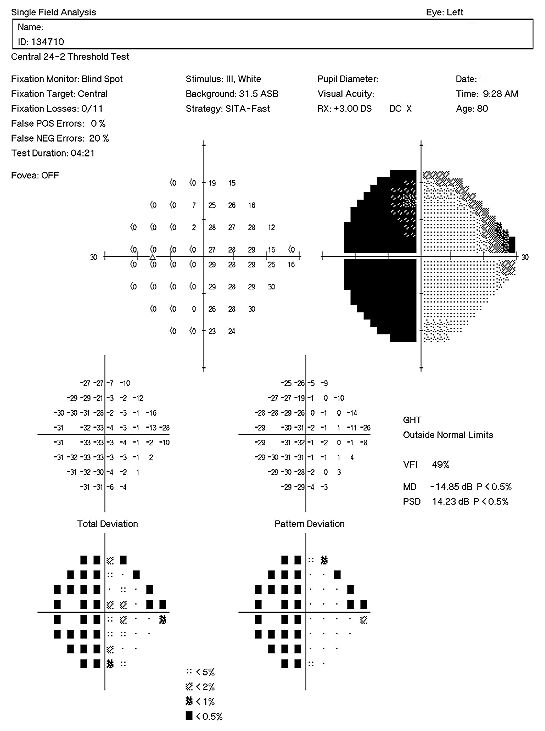
Visual Field Examination
- Various visual field defects will be present depending on the cause
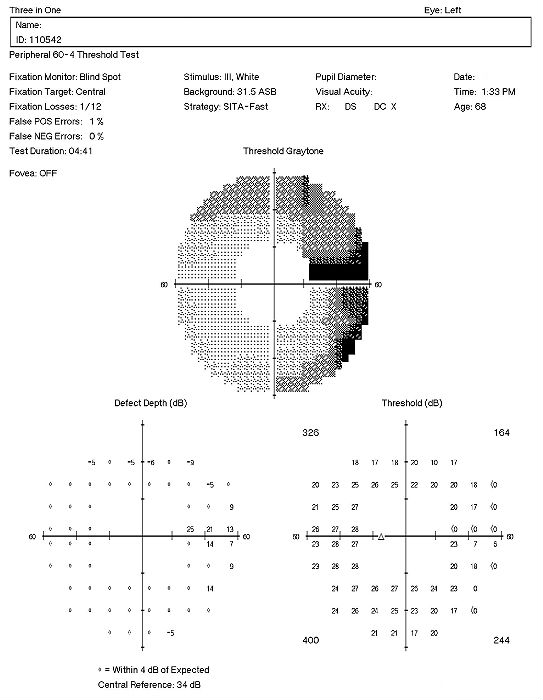
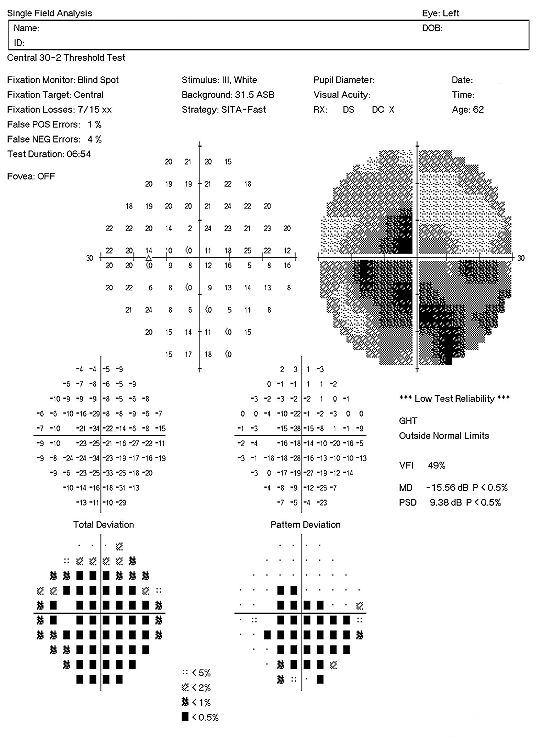 |
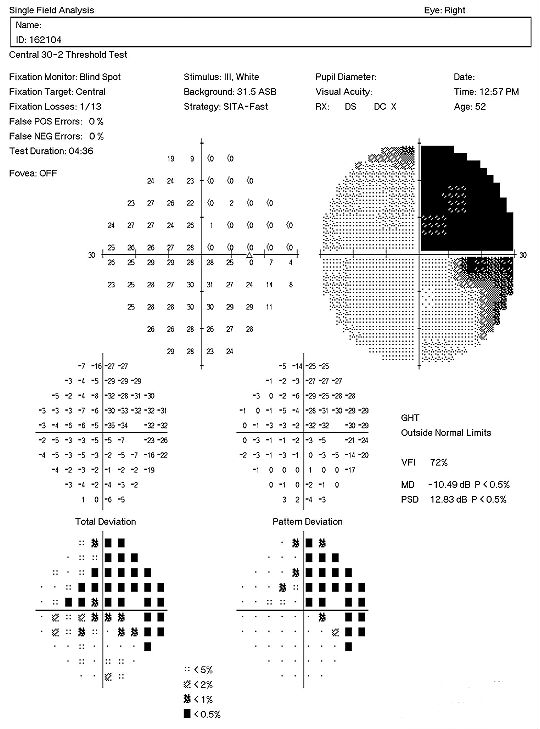
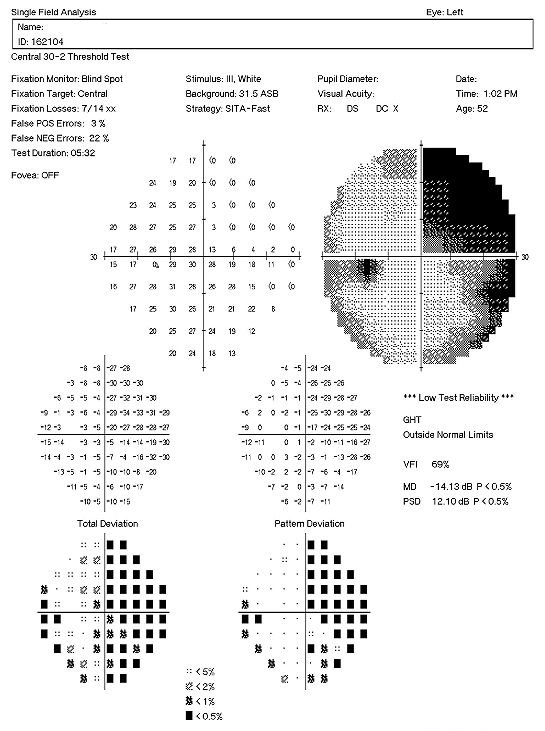
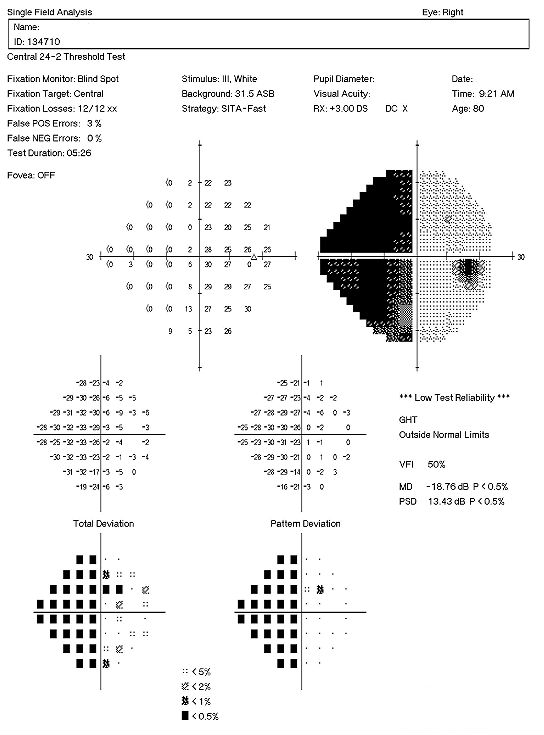
30-2 Threshold Visual Field Examination
|
Extended Ophthalmoscopy
- Evaluate optic disc morphology
- Document abnormal structural changes to the optic disc
- Evaluate the retina and document abnormalities to the retina and the retinal vasculature
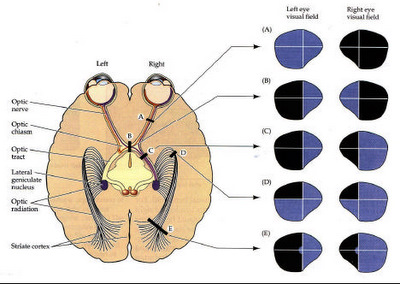
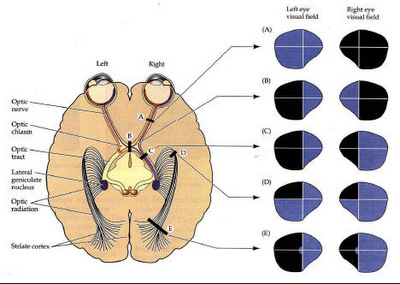
There are several types of visual field defects:
Arcuate scotomas refer to loss of vision around the optic nerve and tend to be related to glaucoma.
Nasal step scotomas refer to loss of vision around the area of the optic nerve and tend to be related to glaucoma.
 |
 |
Central Scotoma refers to loss of vision centrally and can be associated with macular degeneration, macular edema and central serous detachments are a few causes.
Altitudinal Defects refer to loss of vision above or below the horizontal and tend to be associated with ocular abnormalities or vascular disease.
 |
 |
Heteronymous Hemianopia refers to loss of vision on the opposite sides of both eyes and tends to be associated with defects before or at the optic chiasm. A visual field examination showing a visual defect of the temporal side is refered to as\ a bitemporal hemianopia. A visual field examination showing a visuals loss of the nasal side is called a binasal hemianopia.
 |
 |
Homonymous Hemianopia refers to loss of vision on one side of both eyes and tends to be associated with defects behind the optic chiasm.
Macular degeneration
- Some patients may have central visual field defects related to the macula.
Retinal Detachments or Tears
- Patient with retinal detachments or tears can also experience visual field defects.
Ocular Migraines
- Some visual disturbances during an ocular migraine can mimic vision and visual field
loss.
Dermatocholasis
- Excessive dermatocholasis can simulate visual field defects on perimetry examination
and perceived visual field loss from the patients perspective
Find out cause of visual field defect and treat according to the cause
Systemic causes related to vascular or neurological issues need to be directed to the patient’s primary care physician to resolve the underlying systemic. Sudden onset of visual field defects requirement immediate action to find the cause, especially if it is vasculature related and to refer if appropriated. Fluorescein angiography may be recommended depending on the cause and referral to a retinal specialist may be appropriate in some cases. Long term on gradual visual field defects can be monitor with visual field examination after the cause is determined.
Eye disease or optic nerve disease should be treated according to the cause of the visual loss. Please refer to the appropriate disease glossary topic related to the cause of the visual field defect for further details on that particular disease.
1. Chaglasian, M. Sharpen Your Visual Field Interpretation Skills. RevOptom. 15 Feb 2013. http://www.revoptom.com/content/c/39563/. Last accessed August 18, 2014.
2. Martel J. Visual Field Exam. Healthline. 7 Aug 2012. http://www.healthline.com/health/visual-field#Overview1. Last accessed August 18, 2014.
3. Digre K, Brennan K.C. Shedding Light on Photophobia. J Neuroophthalmol. March 2012. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3485070/. Last accessed August 27, 2016.
4. Beatty S. Non-Organic Visual Loss. Postgrad Med J 1999;75:201–207. http://pmj.bmj.com/content/75/882/201.full.pdf. Last accessed August 27, 2016.
368.40
Visual field defect, unspecified
92015
Refraction
92083
Visual field examination
95930
Visual evoked potential
92275
Electroretinography
92283
Color vision examination
92133
Retinal nerve Fiber layer scan
92134
Macula OCT scan
Occurrence
- The prevalence of visual field defect is 5% of the population over 40 years old.
Distribution
- Visual field defect are distributed evenly throughout the population.
Risk Factors
- Glaucoma
- Systemic cardiovascular disease (hypertension, strokes, heart attack)
- Diabetes
- Age




 Print | Share
Print | Share