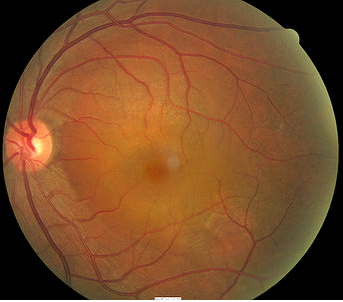
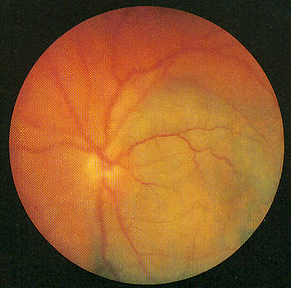
Serous detachment in the macula in
central serous retinopathy
ICD-10 Diagnosis Codes:
H35.711–Central serous chorioretinopathy, right eye
H35.712–Central serous chorioretinopathy, left eye
H35.713–Central serous chorioretinopathy, bilateral
Title
Central Serous Retinopathy
Category
Other Retinal Disorders
Description
A spontaneous serous detachment of the neurosensory retina in the macular region.
Central serous retinopathy involves a breakdown of the outer blood-retinal barrier resulting in a localized detachment of the sensory retina in the macula region. The condition is usually unitateral and occurs secondary to retinal pigment epithelial defect.
Contributing factors to central serous retinopathy include the following:
- Stress
- Excessive alcohol
- Use of inhaled and orally administered steroids
- Uncontrolled hypertension
- Acid reflux
- Cushing disese
- Systemic lupus erythematosus
Structural Damage to the Eye
- A breakdown of the outer blood-retinal barrier alters the physiology of the retinal pigment epithelium
- Focal defects form in the retinal pigment epithelialium
- Sensory retina detaches at the macula
- Unresolved cases lead to progressive retinal pigment epithelium changes
- Prolonged detachment may lead to choroidal neovascular membrane
Functional Damage to the Eye
- Metamorphopsia secondary to macular detachment
- Reduced central visual acuity secondary to macular detachment
- Reduced central visual acuity secondary to progressive retinal pigment epithelium changes
The main goal of the diagnostic evaluation in a patient with central serous retinopathy is to accomplish the following:
- Determine if the etiology is psychological or systemic
- Educate the patient of the cause
- Address or modify any contributing factors
- Prescribe a treatment program to treat the retinal pathology separate from the contributing factor
Patient History
The symptoms of central serous retinopathy vary from no symptoms to severe visual impairment. Patients with early disease my report blurred vision, decreased vision, or mild visual distortion. More advanced presentations often produce metamorphopsia, micropsia, or other abnormal visual distortion of shape and size.
50-year-old Asian male with unilateral decreased vision.
- 20/25 in the right eye
- 20/400 in the left eye
Clinical Appearance of the Retina
- Serous detachment in the left macula without subretinal blood or lipd exudates
- Serous macular detachment is characterized by sloping margins that gradually merge into the attached retina
 |
 |
DIAGNOSTIC TESTS
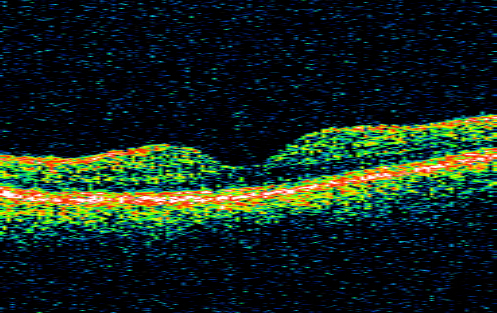
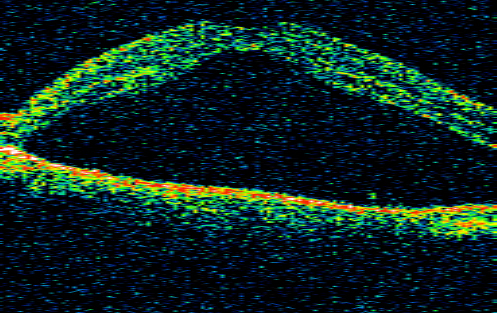
Retinal Scanning Laser — Macula
- Time-domain OCT to detect neurosensory retinal detachment
- Right eye reveals normal foveal structure
- Left eye shows a full-thickness sensory retina detachment
- Sensory retina separated by an optically empty zone from the underlying retinal pigment epithelium
 |
 |
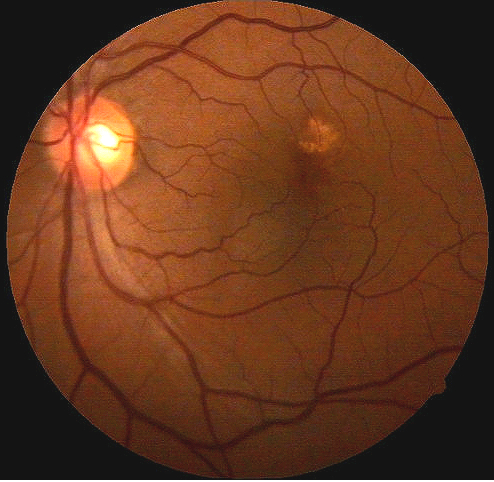
Fluorescein Angiography
- Photographic surveillance of the passage of fluorescein through the retinal and choroidal vasculature
- Smoke-stack appearance is the most common defect pattern seen in central serous retinopathy
- Ink-blot appearance is a less common defect pattern seen in central serous retinopathy
 |
Central Serous Retinopathy
|
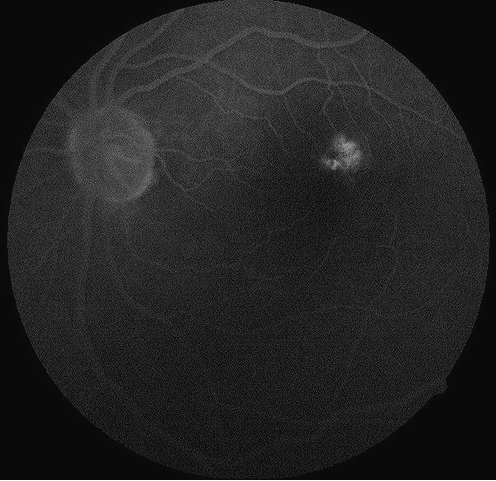 |
Fluorescein Angiogram
|
Although there is no formal classification for central serous retinopathy, the condition may be classified according to its course.
Short-Term Central Serous Retinopathy
- Most common form of the disease
- Spontaneous absorption of subretinal fluid occurs within 3-6 months
- Visual acuity returns to normal or near normal levels
- Recurrences occur in up to 50% of all patients
Prolonged Central Serous Retinopathy
- Condition last longer than 6 months but spontaneously resolves in 12 months
- Some degree of mild visual impairment is possible
Chronic Central Serous Retinopathy
- Least common form of the disease
- Patient is usually over 50-years-old
- Progressive changes in the retinal pigment epithelium
- Moderate-to-severe visual impairment is likely
- Severe cases may develop choroidal neovascularization
This would include any other disease that might produce a serous detachment of the sensory retina in the macular area.
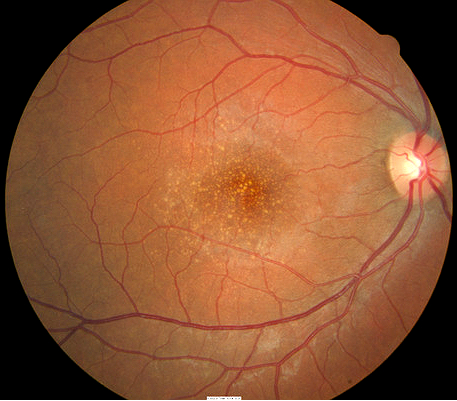 |
Age-Related Macular Degeneration
|
|
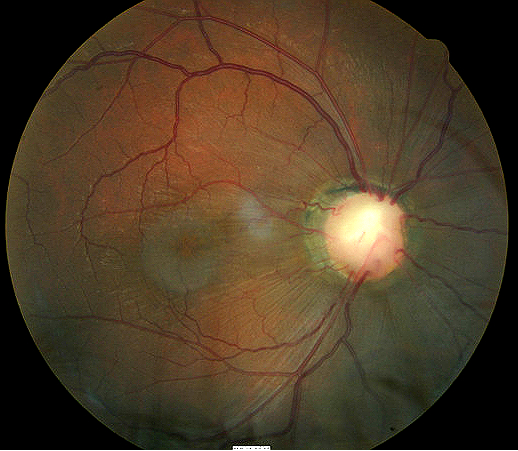 |
Optic Pit
|
|
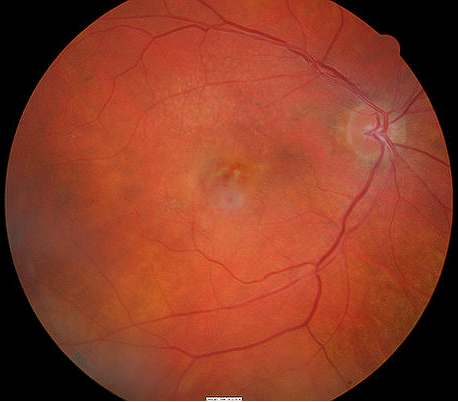 |
Choroidal Neovascular Membrane
|
|
 |
Malignant Choroidal Melanoma
|
Most cases of central serous retinopathy do not require medical or surgical treatment.
Palliative Treatment
- Observation for spontaneous absorption of subretinal fluid
- Examine patient every 6-8 weeks for up to 6 months
- Consider surgical treatment if visual acuity worsens over time
Pharmacologic Treatment
- Discontinue any topical or systemic steroids
Surgical Treatment
Argon Laser Photocoagulation
- Accelerates absorption of subretinal fluid
- Does not improve final visual acuity
- May increase the risk of choroidal neovascularization
- Wait at least 4 months before considering treatment after the first incident
- Consider for prolonged central serous retinopathy
- Consider for recurrent central serous retinopathy
- Patient requires prompt improvement in vision for occupational or psychological needs
- Consider for contralateral eye after poor visual result from a previous episode of central serous retinopathy
Photodynamic Therapy
- May be beneficial in severe cases with choroidal neovascularization
- Consider for chronic central serous retinopathy
1. Shuler K. Diagnosing and Managing Central Serous Chorioretionapthy. American Academy of Ophthalmology. http://www.aao.org/publications/eyenet/200602/pearls.cfm. Last accessed August 17, 2014.
2. Theng K. Central Serous Chorioretinopathy. Medscape/EMedicine. 13 Feb 2013. http://emedicine.medscape.com/article/1227025-overview. Last accessed August 17, 2014.
3. Idiopathic Central Serous CHorioretinopathy. Handbook of Ocular Disease Management. http://www.reviewofoptometry.com/cmsdocuments/2012/6/ro0612_hndbk_em.pdf. Last accessed August 17, 2014.
362.41
Central serous retinopathy
92250
Fundus photography
92225
Extended ophthalmoscopy
92134
Macula OCT scan
92083
Visual Field Examination
92283
Color Vision Examination
92275
Electroretinography




 Print | Share
Print | Share