Case Report ID: 34
Title
Normal-Tension Glaucoma; Abnormal Macular OCT Scan
Category
Glaucoma (8)
Description
This case presents the diagnosis and treatment of normal-tension glaucoma. In normal-tension glaucoma, the intraocular pressure is never measured above 21mm Hg.
Glaucoma is an optic neuropathy showing distinctive changes in optic nerve morphology without associated pallor. The term “glaucoma” refers to a group of chronic, progressive optic neuropathies that have in common characteristic morphologic changes at the optic nerve and retinal nerve fiber layer.
The glaucomas are associated with the following clinical features:
- Aqueous outflow restrictions
- Unphysiologic intraocular pressure
- Abnormal ocular perfusion
- Abnormal rate of apoptosis
- Progressive retinal ganglion cell loss
- Characteristic changes in optic nerve anatomy
Case Report
- 72-year-old black woman presented with a complaint of decreased vision
- Case history described a subjective decrease in vision in the right eye
- The patient had been examined by another eye doctor six months earlier, received new eyeglasses, and wanted to see if another new pair of eyeglasses would improve her vision
Conclusion
Glaucoma is a diagnosis of exclusion. In particular, the diagnosis of normal-tension glaucoma can be difficult. To avoid missing the diagnosis, remember that “normal” intraocular pressure relates to the statistical sense and is no guarantee that the patient does not glaucoma.
Additionally, caution should be exercised in making the diagnosis of normal-tension glaucoma without multiple recordings of intraocular pressure several times during the day. Intraocular pressure can vary dramatically during the twenty-four hour daily cycle, from day-to-day, and when influenced by environmental factors. As thorough an understanding of a patient’s intraocular pressure is essential before beginning any treatment regimen.
History of Present Illness
Associated Symptoms: decreased vision was more bothersome when reading
Location: right eye
Duration: 2 months
Quality: vision is dim
Context: constant
Severity: moderate decrease in vision
Timing: getting worse
Modifiers: none, trying to see if new eyeglasses will help
Review of Systems
The patient reported that she was in good health for her age.
- Past history: non-contributory
- Family history: non-contributory
- Social history: quit smoking ten years earlier
Best Corrected Distance Visual Acuity
- 20/25 in the right eye
- 20/20 in the left eye
Normal Examination Findings
- Mental status
- Intraocular pressure
- Gross medical observation
- Basic sensorimotor examination
- External examination
- Adnexal examination
- External ocular examination with biomicroscopy
Intraocular Pressure Measurements
- 16 mm Hg in the right eye @ 5:00 pm
- 16 mm Hg in the left eye @ 5:00 pm
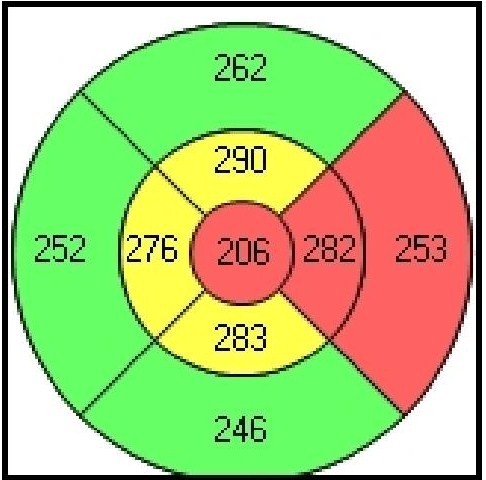
Gross Visual Fields
- A constriction in the superior field of the right eye revealed with confrontation testing
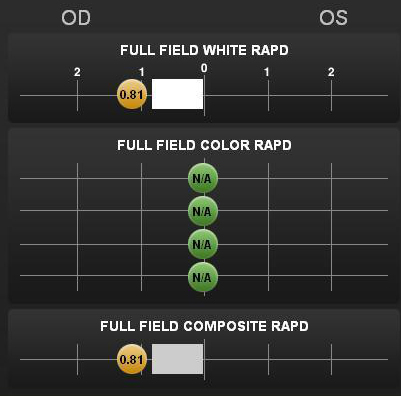
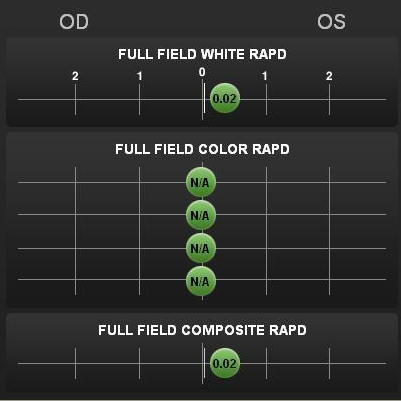
Pupillary Examination
Pupillary reactivity testing using a RAPDx automated pupillographer was abnormal.
- A relative afferent pupillary defect was detected in the right eye
- Index of defect number was 0.81 for the amplitude of the pupillary response in the right eye
- Numbers is calculated by determining the log of the difference in amplitude between the pupillary responses
- Numbers above 0.30 are considered abnormal
- Higher the number, the more likely pathology is present in the neural light reflex pathway
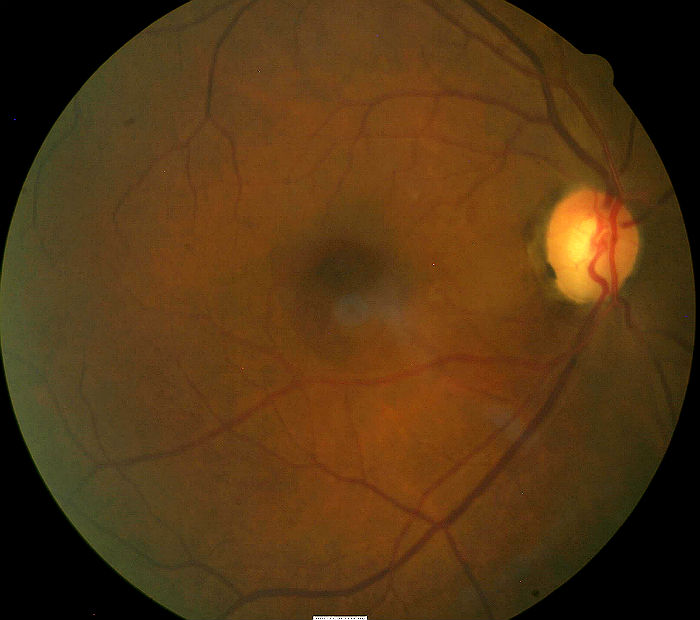
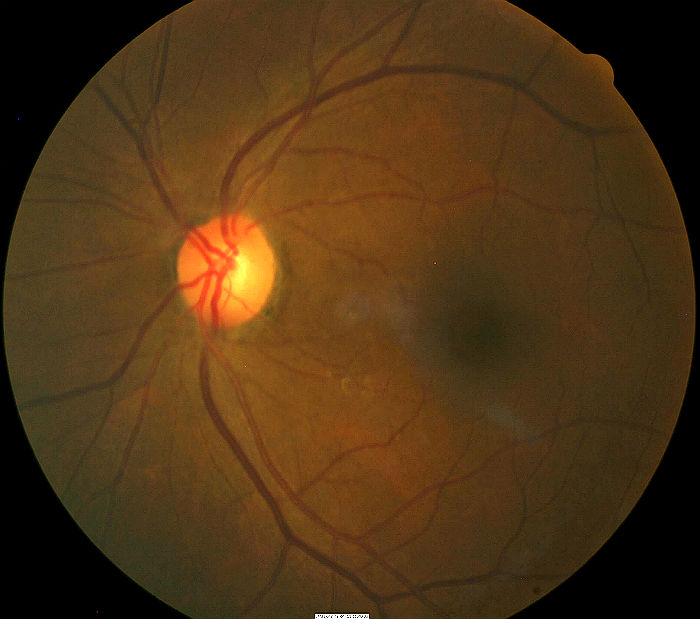
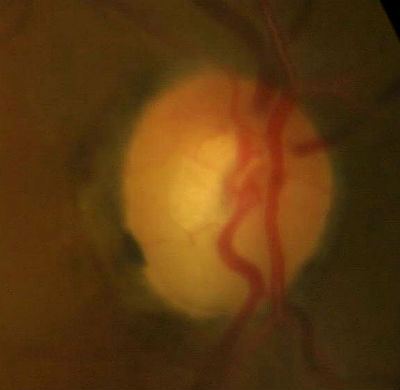
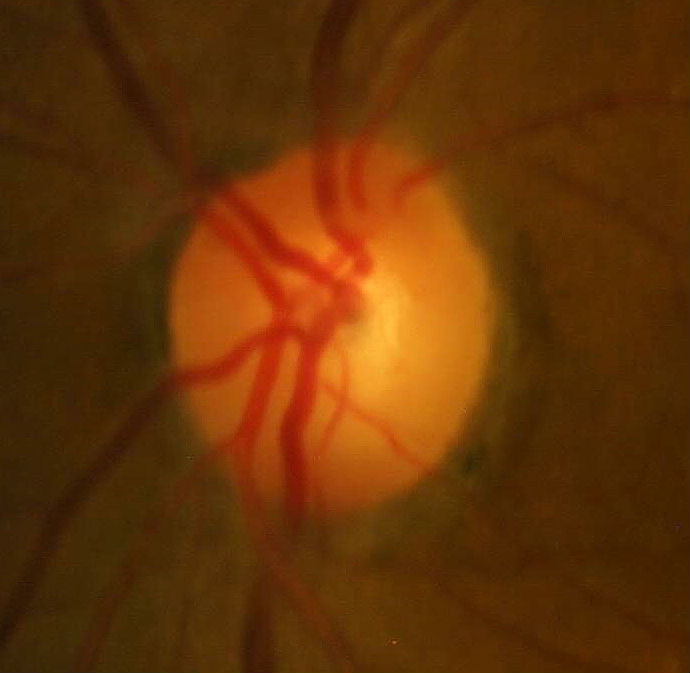
Ophthalmoscopy
The evaluation of the retina and the optic nerve was abnormal.
- Cup-to-disc ratio = .75/.80 in the right eye
- Cup-to-disc ratio = .70/.65 in the left eye
- Peripapillary atrophy in both eyes
Clinical Diagnosis
The clinical diagnosis is determined based on the knowledge obtained fro the patient’s medical history and from the results of the eye examination alone, without the benefit of diagnostic tests or procedures.
The patient’s clinical disgnosis is normal-tension open-angle glaucoma based on the following clinical findings:
- Optic neuropathy in the right eye
- Relative afferent pupillary defect in the right eye
- Visual field defect in the right eye
Treatment Plan
To gather the clinical information required to treat normal-tension open-angle glaucoma, a diagnostic and treatment program is initiated.
- Determination of different types of diagnoses
- Selection of one or more treatment options
After a clinical diagnosis has been determined, the diagnostic process continues with a process that involves the identification and exclusion of differential diagnoses. The differential diagnosis process allows the eye doctor to distinguish between two or more diseases with similar signs and symptoms by systematically comparing their signs and symptoms.
Differential Diagnoses
Much like glaucoma, the first differential diagnosis that needs to be determined in this patient is showing any glaucomatous optic neuropathy versus some other retinal or neurological disease. The list of possible differential diseases would include:
-
Retinal detachment
-
Pituitary tumors and other neurological conditions
-
Ischemic optic neuropathy
-
Vascular disease
-
Drusen of the optic disc
-
Congenital disc anomalies
Diagnostic Testing
When additional clinical information is needed to complete the differential diagnostic process, diagnostic tests and procedures are ordered.
The performance of these tests and procedures leads to the completion of the differential diagnostic process while simultaneously initiating the treatment program. Based on the clinical diagnosis of glaucoma suspect, the following diagnostic tests and procedures might be considered at the conclusion of the eye examination.
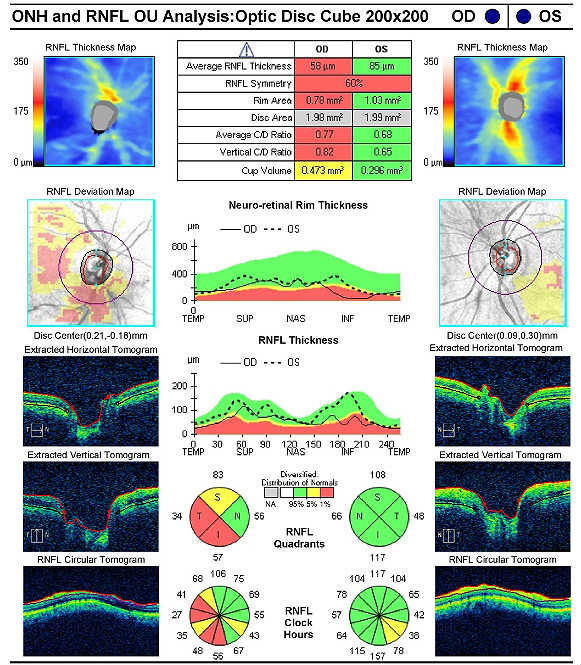
- Retinal nerve fiber layer scan
- Visual field examination
- Gonioscopy
- Fundus photography
- Visual evoked potential
- Electroretinography
- Serial tonometry
The decision to order and perform additional testing is totally based on the concept of medical necessity which can only be determined by the examining optometrist or ophthalmologist.
After a clinical diagnosis has been determined, the diagnostic process continues with a process that involves the identification and exclusion of differential diagnoses. The differential diagnosis process allows the eye doctor to distinguish between two or more diseases with similar signs and symptoms by systematically comparing their signs and symptoms.
Differential Diagnoses
The first differential that needs to be determined in this patient is glaucoma vs. some other retinal or neurologic disease. The list of possible diseases would include any pathology that produces an asymmetric partial optic atrophy and a relative afferent pupillary defect in the same eye.
The following diseases share some of the clinical signs and symptoms of glaucoma:
-
Retinal detachment
-
Pituitary tumors and other neurological conditions
-
Ischemic optic neuropathy
-
Vascular disease
-
Drusen of the optic disc
-
Congenital disc anomalies
Retinal detachments and drusen of the optic disc would be easily identified during routine ophthalmoscopy. Pituitary tumors producing morphologic changes in the optic nerve should be associated with characteristic bitemporal visual field defects. The patient did not have a history of vascular disease and no retinal vascular findings that would typically be associated with more advanced systemic vascular disease.
Diagnostic Testing
When additional clinical information is needed to complete the differential diagnostic process, diagnostic tests and procedures are ordered.
The performance of these tests and procedures leads to the completion of the differential diagnostic process while simultaneously initiating the treatment program. Based on the clinical diagnosis of glaucoma suspect, the following diagnostic tests and procedures might be considered at the conclusion of the eye examination.
- Retinal nerve fiber layer scan
- Visual field examination
- Gonioscopy
- Fundus photography
- Visual evoked potential
- Electroretinography
- Serial tonometry
The decision to order and perform additional testing is totally based on the concept of medical necessity which can only be determined by the examining optometrist or ophthalmologist.
INITIAL EXAMINATION – DAY 1
Refraction
- Measuring visual acuity is a method of evaluating functional vision loss
- Advanced glaucoma can produce central visual field defects which result in a loss of visual acuity
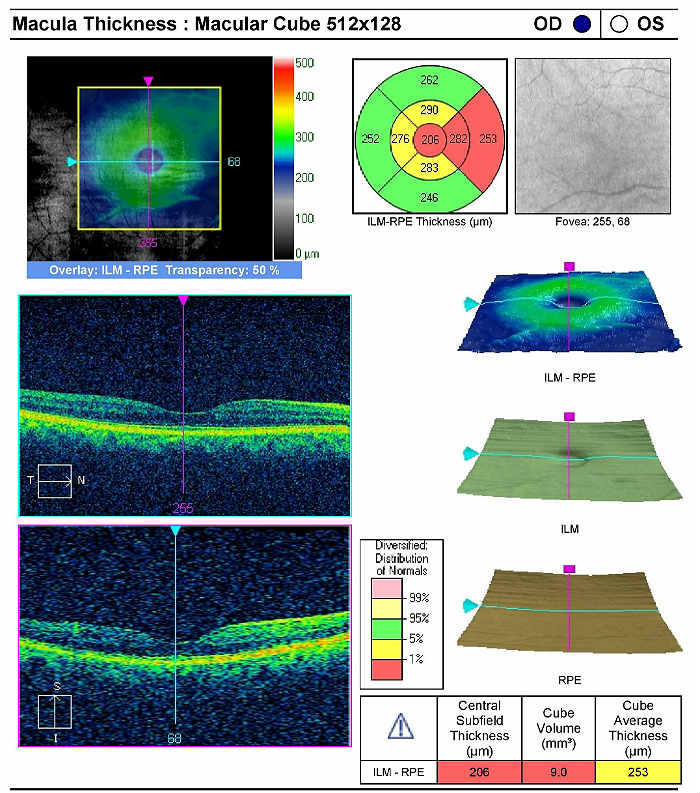
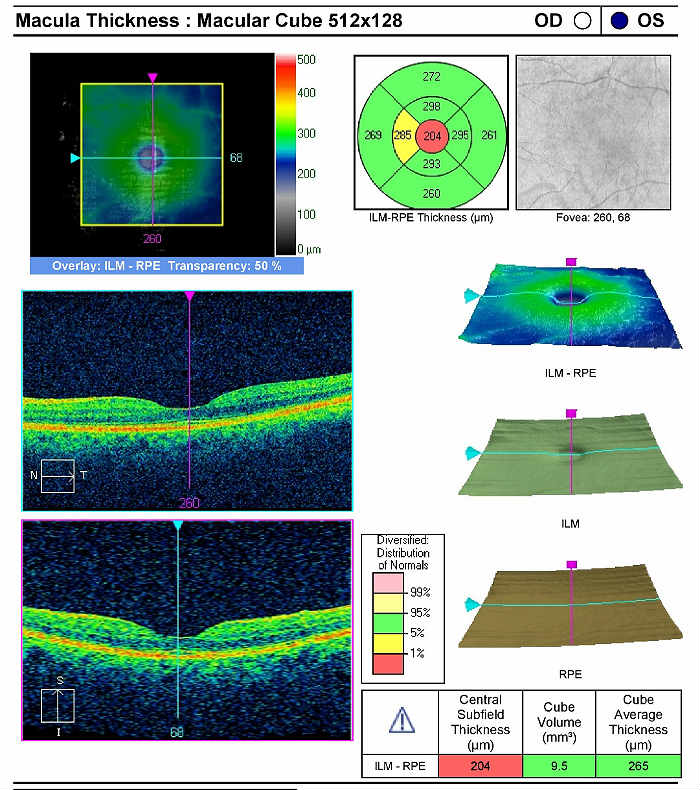
Retinal Laser Scan — Nerve Fiber Layer
- Measuring the average retinal nerve fiber layer thickness provides an overall assessment of retinal health
- The procedure can be accomplished by using the Cirrus OCT manufactured by Carl Zeiss Meditec
Retinal Laser Scan — Macula
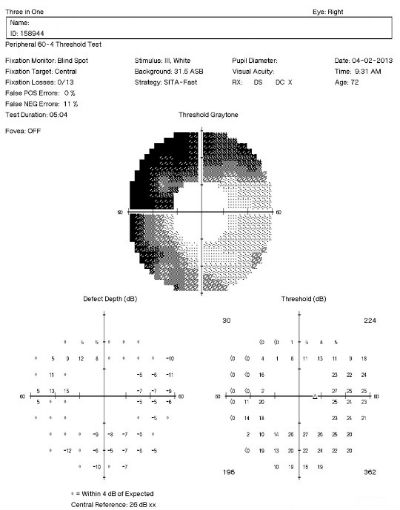
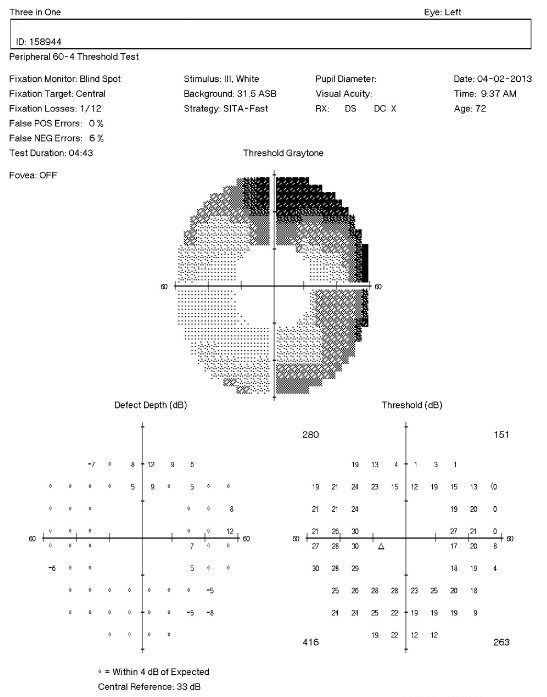
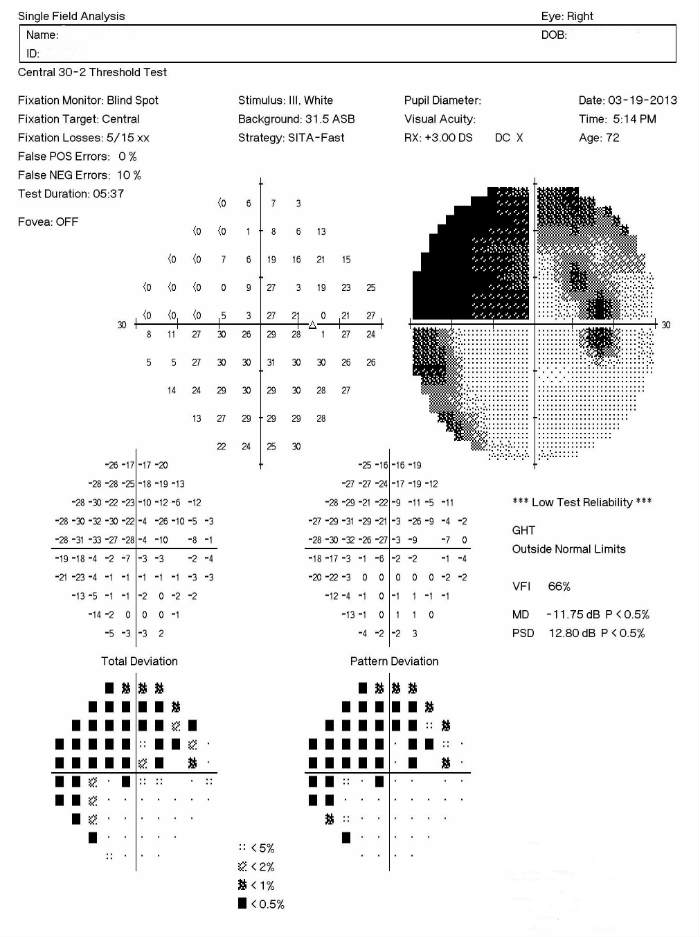
Visual Field Examination
- Automated threshold perimeters measure the visual field by plotting the threshold luminance value of the patient in various locations in the visual field
- The luminance of the light stimulus is represented by non-specific units of measurement called decibels (dB)
- Glaucoma produces several changes in the visual field, and one of these changes occurs as a widespread, non-descript loss of retinal sensitivity
- In Tranquair’s “Hill of Vision” concept, loss of retinal sensitivity represents a reduction in the height of the hill
- The diffuse loss of retinal sensitivity should be considered highly diagnostic of glaucoma when it is asymmetric and correlates with asymmetric changes in intraocular pressure or disc appearance
- In most cases, the loss of sensitivity occurs in characteristic patterns and locations (e.g., nasal step, arcuate scotoma, paracentral scotoma) that often correlate with changes in the optic nerve and/or retinal nerve fiber layer.
 |
 |
Automated threshold perimeters characterize specific parameters of the overall visual field status by the use of numbers called Global Indices. One of the indices, Mean Deviation (MD), expresses the raw data generated by the instrument.
A visual field defect can be classified as mild, moderate or advanced based upon an abnormal Mean Deviation.
- Mild visual field defect = 0 through -5.99 dB
- Moderate visual field defect = -6.00 dB through -11.99 dB
- Advanced visual field defect = anything above -12.00 dB
Right Eye
- Severe loss of retinal sensitivity
- Incomplete superior arcuate scotoma
- Enlarged blind spot
- Marginal test reliability
- Visual field defect appears to be a horizontal and vertical respect of the midline
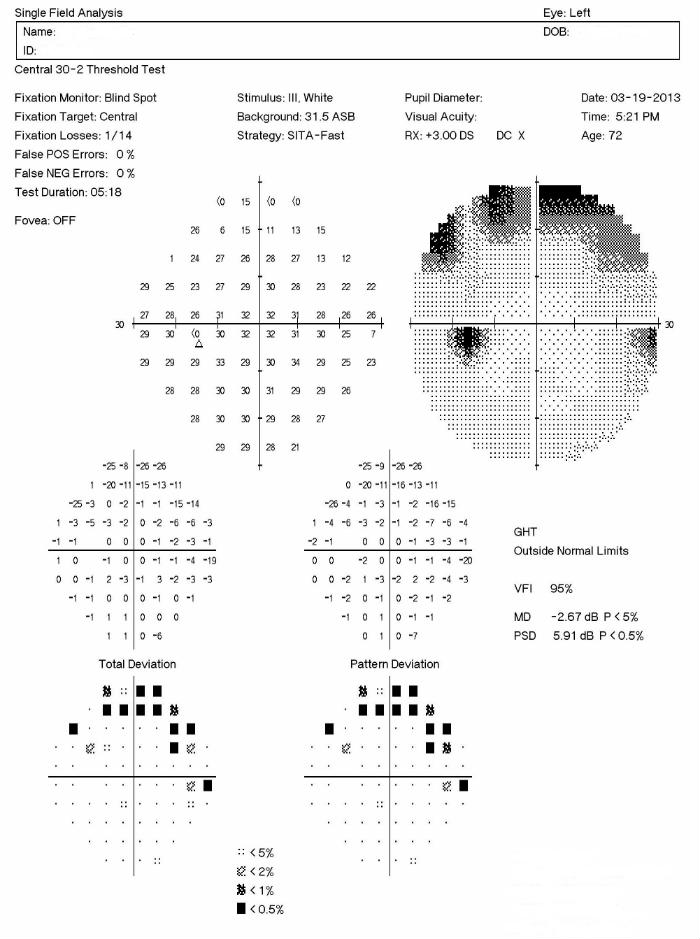
Left Eye
- Mild loss of retinal sensitivity
- Incomplete superior arcuate scotoma
- Normal blind spot
- Good test reliability
Both Eyes
- Asymmetric loss of retinal sensitivity
Because of the apparent respect of the midline, the etiology of the visual field defect in the right eye could be neurologic in origin. As a result, an MRI of the brain with contrast was ordered.
SUBSEQUENT ENCOUNTER — DAY 14
Magnetic Resonance Imaging (MRI)
One day after the eye examination, an MRI without and with intravenous gadolinium was performed at a nearby imaging center. There was no prior examination for comparison.
Radiologist’s Findings:
- There is no restricted diffusion to suggest recent infarction
- There is no intracranial mass effect or midline shift
- The ventricular system, sulci, and cisterns are normal in size and morphology
- No brain parenchymal signal abnormality or abnormal enhancement is demonstrated
- No orbital mass or optic nerve enhancement is demonstrated
- Sinuses and mastoids are clear
- There are scattered T2 hyperintensities in the supratentorial white matter and brainstem
Radiologist’s Impression:
- No acute intracranial abnormality
- No enhancing mass lesion or recent infarct
- T2 hyperintensities are most compatible with chronic small vessel ischemia, particularly given the patient’s age
Physical Diagnosis
A lesion of the lateral geniculate nucleus near the sulcus could produce the visual field defect seen in the right eye, but it should have been revealed on the MRI examination. Because of this, the differential diagnosis of neurologic disease was excluded and the clinical diagnosis of normal-tension glaucoma was confirmed.
Visual Field Examination
A 60-4 testing strategy sometimes gives a different perspective compared to traditional 30-2 field examinations.
Right Eye
- Superior arcuate scotoma
- Good test reliability
Left Eye
- Superior arcuate scotoma
- Good test reliability
Both Eyes
- Clinically significant asymmetry correlates with abnormal OCT test results, abnormal RAPDx automated pupillography and decreased visual acuity in the right eye
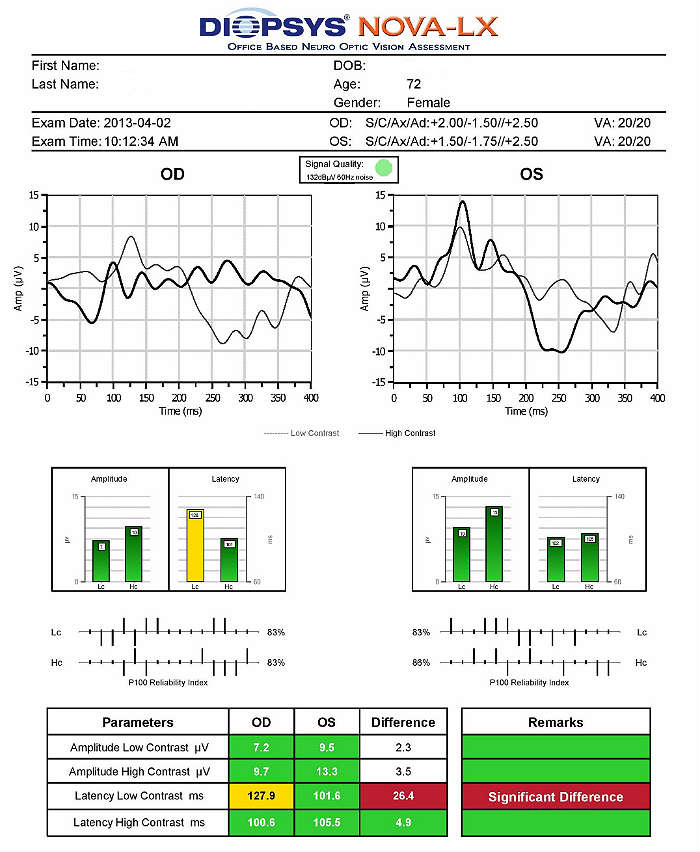
Visual Evoked Potential Testing
The VEP is an objective electric sign of visual pathway function and its parameters are sensitive to abnormalities in the visual system. By measuring the speed and strength of the neural responses along the visual pathway, VEP testing evaluates the integrity of the afferent visual sensory system.
- Abnormal waveform peak latencies and shape helps to identify pathologies ranging from the eye through the brain to the primary visual cortex
- The procedure can be accomplished with the NOVA-LX VEP Testing Device manufactured by DIOPSYS
Measuring the conduction speed and magnitude of the neural response from the eye to the cortex can be helpful in assessing early changes in glaucoma. Although not diagnostic of glaucoma, abnormal VEP test results in addition to other abnormal clinical findings can assist in making the difficult diagnosis of early glaucomatous damage.
All of the diagnostic test results confirmed the clinical diagnosis of normal-tension open-angle glaucoma, although this diagnosis may change with additional trending of intraocular pressure. Additional diagnostic tests for glaucoma such as serial tonometry, provocative glaucoma testing, gonioscopy or extended ophthalmoscopy were not considered medically necessary on this patient’s last two visits. Photographic documentation of the optic nerve would be an additional medically necessary test that could be obtained at any follow-up examination.
According to Current Procedural Terminology, when eye doctors perform ophthalmological examinations, the complexity of medical decision-making is not separated from the examining techniques used. As a guideline to assist eye doctors in enhancing their medical decision-making skills, consider that the complexity of medical decision-making involves three components.
The first component concerns the number of possible diagnoses and treatment options that must be considered. Modern glaucoma diagnosis involves the determination of structural damage to the eye and/or functional loss to the visual system. Once these assessments are made, the glaucoma must be classified by type and ICD-9 lists multiple designations of glaucoma suspect (ICD-10 includes many more). The most specific diagnosis in this case would be 365.12, low-tension glaucoma.
The second component concerns the amount and complexity of medical records and diagnostic tests that have to be obtained, reviewed and analyzed. In addition to an eye examination, this visit required the review and analysis of a subjective refraction, a retinal laser scan and a threshold visual field examination. In addition, an MRI of the brain was ordered for the next day. Also, orders were entered into the medical record to perform a confirmatory visual field examination and visual evoked potential testing at the next visit.
Third, the complexity of medical decision-making is affected by the risk of significant complications and/or morbidity associated with mild glaucoma and the risks involved in any treatment options. This patient’s glaucoma was classified as a significant problem where the risk of total vision loss without treatment was possible. In addition, because the treatment plan would involve chronic pharmaceutical treatment with the potential for ocular and systemic side effects, the pharmacology complications had to be considered when deciding on the initial treatment options.
Treatment Guidelines
To begin the treatment of glaucoma, intraocular pressure must be lowered and an initial target pressure range must be established. A general guideline is to base the initial pressure range on the category of damage to the visual system.
- Mild damage needs a 20-30% reduction in pre-treatment IOP as the initial target pressure range
- Moderate damage needs a 30-40% reduction in pre-treatment IOP as the initial target pressure range
- Advanced damage needs a 40-50% reduction in pre-treatment IOP as the initial target pressure range
Doctors should always remember that the goal of glaucoma therapy is to prevent additional or future vision loss, not achieve some arbitrary target therapy range.
Due to the advanced glaucomatous damage to the right eye, a 40-50% reduction in the pre-treatment intraocular pressure was selected as the initial target pressure range.
Treatment Program
Modern glaucoma therapy generally utilizes prostaglandins as the primary therapy. The first goal of treating glaucoma is to achieve the lowest possible IOP on a single agent and prostaglandins generally have the greatest efficacy of all glaucoma medications.
Monotherapy with prostaglandins improves patient compliance, may decrease costs, and improves the safety profile and tolerability of using topical medications. These drugs reduce intraocular pressure by increasing uveoscleral outflow. IOP reduction averages almost 30% with some patients showing even greater response but a small percentage showing minimal to no response.
Monotherapy with combination medications such as Combigan (Allergan, Inc.) is another primary therapy.
Avoiding medicolegal liability if complications arise is an important part of modern ophthalmic practice. This avoidance is best accomplished by making sure that you have obtained the patient’s informed consent to treat their glaucoma. Once you have made the patient fully aware that using topical glaucoma medicine involves the risks of side effects, you can proceed with the treatment plan.
After obtaining the patient’s informed consent to treat her glaucoma, Combigan ophthalmic solution was prescribed 1 drop twice daily in both eyes.
A target pressure range of 8-10 mm Hg was established for each eye.
Next visit scheduled for three weeks.
Discussion
This case demonstrates several key aspects of treating a patient with an initial diagnosis of normal-tension open-angle glaucoma. On initial examination, the damage to the optic disc and the loss of visual field was advanced in both eyes. The glaucomatous damage in the right eye’s visual system was more advanced and the intraocular pressure was never measured above 16 mm Hg in either eye.
- First, no additional or second opinions are required. Even thought there was advanced damage in the right eye, there was no ocular emergency and no need for a referral to a glaucoma sub-specialist at this time.
- Second, this patient’s clinical history supports the modern understanding of the pathophysiology of glaucoma. We know that glaucoma is an optic neuropathy. Structural damage to the retinal nerve fiber layer is usually the first milestone in the natural history of glaucoma. The loss of retinal nerve fibers is closely followed by changes in the appearance of the optic disc.
- Third, functional loss, which is documented by abnormal visual field testing, abnormal visual evoked potential testing, abnormal pupil reactivity, abnormal color vision or loss of visual acuity, usually occurs later in the natural history of the disease. This case demonstrates that the patient’s glaucoma could have been easily missed without the benefit of automated pupillography.
- Fourth, even though elevated intraocular pressure is a risk factor for glaucoma, we must always be mindful that the glaucomas are a family of diseases characterized by optic neuropathy – not elevated intraocular pressure.
Baltimore Eye Study
- This patient was examined by another eye doctor in another practice six months earlier.
The findings from the Baltimore Eye Study are still true. One of the findings from the Baltimore Eye Study is that glaucoma can be hard to diagnose. The study revealed that 50% of all people found to have glaucoma during the study had seen an eye doctor within the past year and were unaware that they had glaucoma. This failure to diagnose glaucoma is most explained by a function of concentrating on intraocular pressure as a diagnostic indicator as opposed to the appearance of the optic disc.
Early Manifest Glaucoma Trial
Regarding intraocular pressures as a diagnostic indicator, the Early Manifest Glaucoma Trial demonstrated that there is considerable variability of the intraocular pressures in patients with glaucoma. The study also determined that 20-35% of glaucoma patients do not have elevated intraocular pressures. In this group of patients, the intraocular pressure will consistently measure below 21 mm Hg. In addition, the study demonstrated that 50% of patients with glaucoma – even if they had elevated intraocular pressures most of the time – had screening intraocular pressures below 22 mm Hg.
Based on the patient history, the nature of the presenting problem, and my own clinical judgement this patient needed an evaluation of the complete visual system.
- Perform the eye examination that is medically necessary
- Provide the diagnostic tests or services that are medically necessary
- Properly document the services provided
- Code from the documentation
- Report the services to the payor
Physicians Quality Reporting System
PQRS Measure 12: Primary Open-Angle Glaucoma: Optic Nerve Evaluation – CPT code 2027F
This measure applies to patients 18 years and older diagnosed with primary open-angle glaucoma. CPT code 2027F is reported when these patients receive an optic nerve examination. The measure should be reported on the date of the examination and on all subsequent eye examinations during the next 12 months – even if an optic nerve examination was not performed on the follow-up examinations. Remember that you may be required to report this measure more than once since the reporting period covers 12 months.
PQRS Measure 226: Patient screened for tobacco use and identified as a non-user of tobacco – CPT code 1036F
This measure applies to patients 18 years and older. The measure should be reported on the day of the examination and can be used with any diagnosis code.
PQRS Measure 130: Current Medicatons with Name, Dosage, Frequency and Route Documented – CPT code G8427
This measure applies to patients 18 years and older. The measure should be reported on the day of the examination and can be used with any diagnosis code.
Multiple Procedure Payment Reduction
Effective January 1, 2013, there is a small reduction in payment from Medicare if certain multiple procedures are billed on the same day. The fee for the technical component of the diagnostic test for the second and subsequent tests will be reduced by 20%. The second diagnostic test and subsequent tests should be reported with a -51 modifier. Professional services such as gonioscopy, extended ophthalmoscopy and provocative glaucoma testing are excluded from this policy. Visual evoked potential testing is excluded from this policy.
Modifier 51
This modifier is used to identify the secondary procedure or when multiple procedures are performed on the same day by the same provider. List the major primary procedure first and append the modifier to the subsequent procedures. The primary procedure is the one with the highest dollar value.
INITIAL EXAMINATION – DAY 1
| Diagnosis Code | Procedure Code | Modifier | Quantity | Payor | Amount Allowed |
| H40.1213 - Low-tension glaucoma, right eye, severe stage | 92004 - Medical eye examination | 1 | Medicare | 152.38 | |
| H40.1213 - Low-tension glaucoma, right eye, severe stage | 92083 - Visual field examination | 1 | Medicare | 65.76 | |
| H40.1213 - Low-tension glaucoma, right eye, severe stage | 92133 - Retinal laser scan | 51 | 1 | Medicare | 42.19 |
| H40.1213 - Low-tension glaucoma, right eye, severe stage | G8427 - Medications documented | Medicare | 0.00 | ||
| H40.1213 - Low-tension glaucoma, right eye, severe stage | 2027F - Optic nerve evaluation | Medicare | 0.00 | ||
| H40.1213 - Low-tension glaucoma, right eye, severe stage | 1036F - Patient screened for tobacco use | Medicare | 0.00 | ||
| Total | $260.33 |
SUBSEQUENT ENCOUNTER — DAY 7
| Diagnosis Code | Procedure Code | Modifier | Quantity | Payor | Amount Allowed |
| H40.1213 - Low-tension glaucoma, right eye, severe stage | 92012 - Medical eye examination | 1 | Medicare | 87.69 | |
| H40.1213 - Low-tension glaucoma, right eye, severe stage | 92083 - Visual field examination | 51 | 1 | Medicare | 65.76 |
| H40.1213 - Low-tension glaucoma, right eye, severe stage | 95930 - Visual evoked potential | 1 | Medicare | 133.41 | |
| H40.1213 - Low-tension glaucoma, right eye, severe stage | G8427 - Medications documented | Medicare | 0.00 | ||
| H40.1213 - Low-tension glaucoma, right eye, severe stage | 2027F - Optic nerve evaluation | Medicare | 0.00 | ||
| H40.1213 - Low-tension glaucoma, right eye, severe stage | 1036F - Patient screened for tobacco use | Medicare | 0.00 | ||
| Total for both visits | $547.19 |
H40.1213
Low-tension glaucoma, right eye,
severe stage
H40.1222
Low-tension glaucoma, left eye
moderate stage
365.12
Low-tension glaucoma
92133
Retinal laser scan
92250
Fundus photography
95930
Visual evoked potential
92275
Electroretinography
92225
Extended ophthalmoscopy
76514
Corneal pachymetry
92020
Gonioscopy




 Print | Share
Print | Share