ICD-10 Diagnosis Codes:
H20.011–Primary iridocyclitis, right eye
H20.012–Primary iridocyclitis, left eye
H20.013–Primary iridocyclitis, bilateral
Title
Primary Iridocyclitis
Category
Disorders Of The Iris And Ciliary Body
Description
Iridocyclitis is an inflammation of the uvela tissues, primarily the iris and ciliary body.
Primary iridocyclitis is also know as uveitis. It represents an inflammation of the uveal tissues, primarily the iris and the ciliary body and is associated with the following conditions:
- Underlying systemic disease
- Autoimmunity
- Ocular trauma
- Contact lens wear
- Infectious corneal ulcers
- Contact lens-induced hypoxia (CLARE)
Structural Damage to the Eye
- Corneal clouding (edema)
- Cystoid macular edema
- Band keratopathy
Functional Damage to the Eye
- Visual acuity is unaffected
- Visual acuity is partially affected
- Visual acuity is severely affected
The main goal of the diagnostic evaluation of a patient with primary iridocyclitis (e.g., uveitis) is to accomplish the following:
- Determine the extend of the structural damage in the retina
- Isolate any potential risk for retinal detachment
- Determine a monitoring or treatment regimen
Patient History
Most patients with uveitis are asymptomatic unless they experience a complication such as a retinal detachment then they will experience the following symptoms:
- Visual disturbances (such as flashes and/or floaters)
- Black curtain or film cover their visual field
- Sudden vision loss
Intraocular Pressure
Abnormal clinical signs include intraocular pressure in any of the following presentations:
- IOP above 22 mm Hg as measured by applanation tonometry
- Measurements above 24 mm Hg are clinically significant
- 99.85% of the population have IOPs below 24 mm Hg
- Increase in IOP over time
- Asymmetric > 5 mm Hg
- Diurnal variation > 6 mm Hg
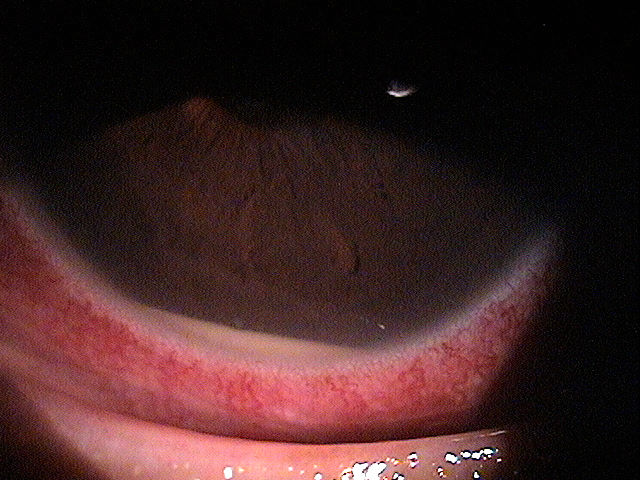
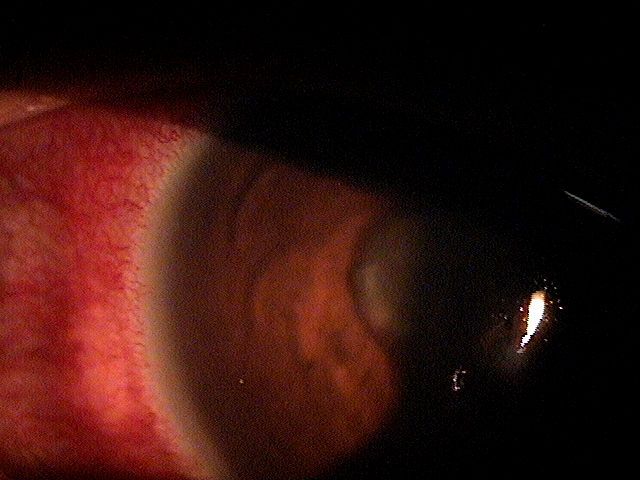
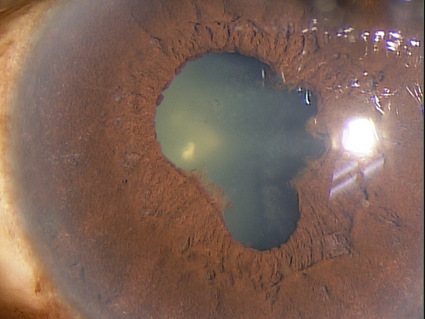
External Ocular Examination with Biomicroscopy
Abnormal clinical signs in the anterior chamber that are associated with uveitis:
- Cells within the anterior chamber secondary to inflammatory cellular infiltration
- Flare within the anterior chamber due to an influx of proteins
- Evaluate cells and flare under high magnification (slit-beam should be 1mm by 1mm at a 45-60 degree angle)
- Hypopyon formation
Abnormal clinical signs in the conjunctiva that are associated with uveitis:
- Perilimbal vessel engorgement (ciliary flush)
- Diffuse hyperemia
Abnormal clinical signs in the cornea that are associated with uveitis:
- Keratic precipitates
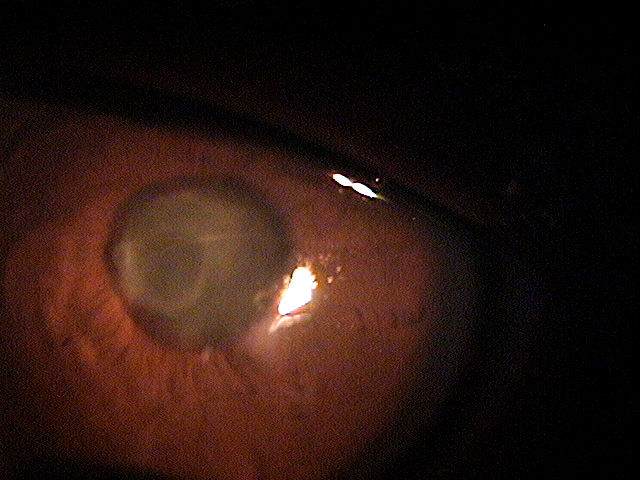
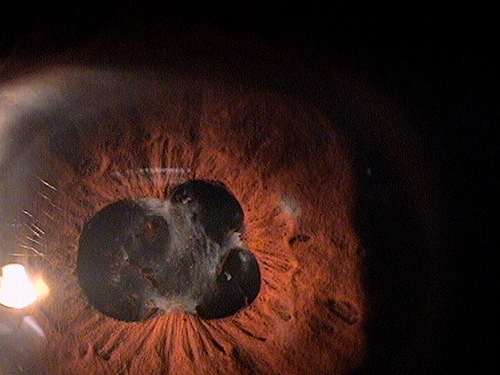
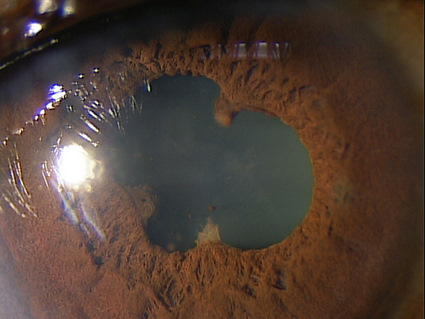
Abnormal clinical signs in the iris and pupil that are associated with uveitis:
- Adhesions of the iris to the anterior lens (posterior synechia)
- Adhesions of the iris to the cornea (anterior synechia)
- Fibrin membrane covering the pupil
Ophthalmoscopy
Abnormal clinical signs in the vitreous that are associated with uveitis:
- Snow banking or snow ball formation
Abnormal clinical signs in the posterior chamber that are associated with uveitis:
- Macular edema
- Vasculitis
- Neovascularization
DIAGNOSTIC TESTS
Refraction
- Measuring visual acuity is a method of evaluating functional vision loss
- Anterior uveitis, in both the acute and chronic phases, can produce a loss of visual acuity
Extended Ophthalmoscopy
Extended ophthalmoscopy is indicated when a more detailed examination and documentation of the vitreous and retinal structures is indicated than a doctor would conduct in routine examination of the interior globe. Routine ophthalmoscopy is part of general ophthalmologic services and not reported separately. However, extended ophthalmosocpy is reported separately as an additional, billable diagnostic procedure.
Uveitis presentations, especially when there is potential for systemic disease as a co-morbidity, requires a detailed evaluation of the vitreous and retinal structures to look for vitreous cells, exudative material over the ora (snowbanking), cellular material in the vitreous (snowballs), vascular sheathing, peripheral neovascularization and retinal detachment.
In many cases, the degree of presenting photophobia may warrant delaying a more detailed internal evaluation to a follow-up visit, but this evaluation should never be eliminated from the diagnostic evaluation.
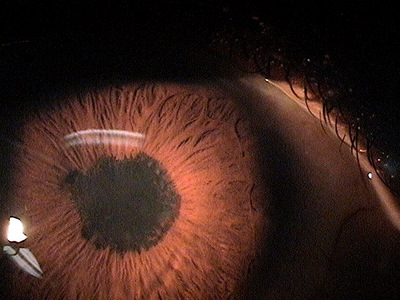
External Ocular Photography
Photodocumentation is considered medically necessary when it provides the doctor with a useful tool for assistance in making the clinical diagnosis or assists in monitoring the disease progression or effectiveness of therapeutic intervention. Anterior uveitis, especially with tissue changes demonstrating disease chronicity and potential for secondary complications, is a sight threatening disorder. Photodocumentation of the current tissue changes could easily be considered as medically necessary.
 |
 |
Retinal Laser Scan – Nerve Fiber Layer
- Measuring the average retinal nerve fiber layer thickness provides an overall assessment of retinal health
- The procedure can be accomplished by using the Stratus OCT manufactured by Carl Zeiss Meditec as well as other scanning lasers
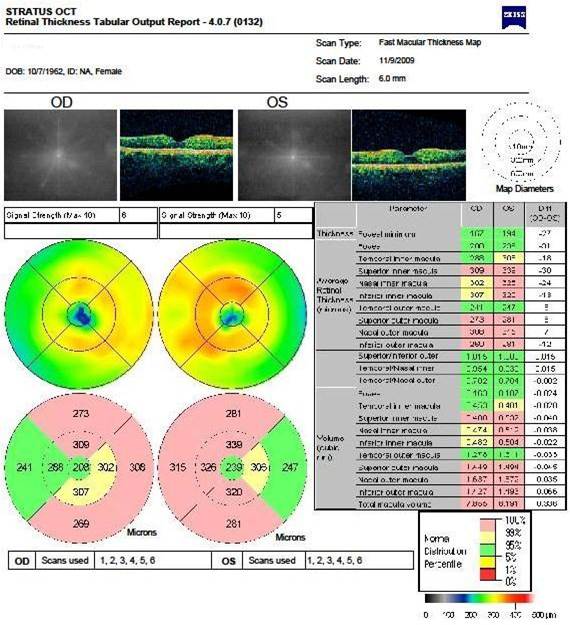 |
Right Eye
|
Specular Endothelial Microscopy
Iridocyclitis can result in endothelial cell loss and reduced endothelial function. The condition is called inflammation-inducedcorneal endotheliopathy and is characterized by the following clinical features:
- Specular microscopy reveals well-demarcated, dark structures usually located at endothelial cell intersections
- These dark structures are thought to represent invading white blood cells (e.g., inflammatory cells)
- Migration of inflammatory cells into the cornea from the anterior chamber produces a sloughing of the endothelium
- More aggressive and/or earlier treatment of any anterior segment inflammation with topical steroids may help with prevention of inflammation-induced endotheliopathy
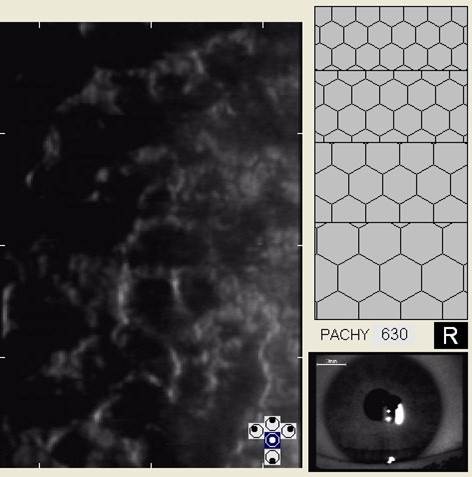 |
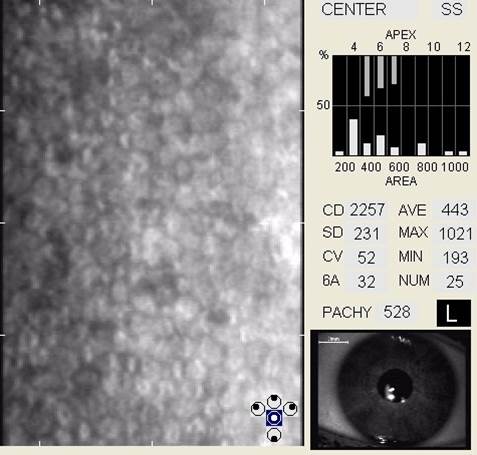 |
B-Scan Ophthalmic Ultrasound
The clinical application of B-scan ophthalmic ultrasound is the documentation, monitoring and treatment of any pathological conditions that affect the external structures of the eye, the anterior segment of the eye or the posterior segment of the eye.
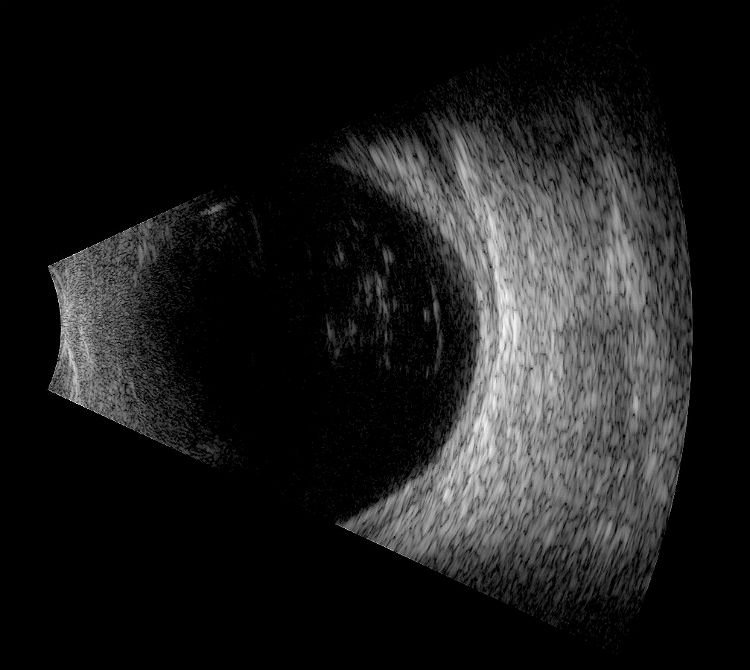 |
B-Scan Ultrasound
|
Uveitis Evaluation / Laboratory Analysis
Eye doctors should not be too quick to suggest a comprehensive systemic evaluation unless truly warranted. Next to trauma, idiopathic etiology is the most common explanation for an acute anterior uveitis. The medical advisability of ordering or referring for a systemic evaluation in patients with anterior uveitis is dependent on several factors including:
- Associated symptoms revealed in a comprehensive review of systems
- History of recurrences
- Presence of clinical findings suggestive of disease chronicity
A basic uveitis work up could include any or all of the following studies, depending on the level of suspicion each analysis could be associated with.
| Diagnostic Test | Suspected Disease Association |
| VDRL (Better FTA-ABS) | Syphilis |
| PPD | Tuberculosis |
| HLA-B27 | Ankylosing spondylitis; idiopathic reactive arthritis; juvenile arthritis |
| RhF | Rheumatoid arthritis |
| LIA | Lyme’s disease |
| ANcA | Wegener’s granulomytosis |
| ANA | Lupus |
| X-ray | Ankylosing spondylitis; rheumatoid arthritis; sarcoid (chest); Lupus |
| Endoscopy / Colonoscopy | Irritable bowel syndromes |
Primary care eye doctors should communicate as specifically as possible regarding their suspicion of systemic involvement in a patient presenting with anterior uveitis. This can and should be as detailed as recommending specific laboratory analysis based on the suspected systemic disease driving the inflammatory process.
The International Uveitis Study Group (IUSG) has four classifications for uveitis based on anatomic location as the primary source of the ocular inflammation:
- Anterior uveitis — starts in the anterior chamber
- Intermediate uveitis — starts in the vitreous
- Posterior uveitis — starts in the retina and choroid
- Panuveitis — no predominate site as the source of inflammation, with involvement in the anterior chamber, vitreous, retina and/or
In addition, the Standardization of Uveitis Nomenclature (SUN) Working Group classifies uveitis by the onset andduration of the inflammatory episodes.
- Sudden onset uveitis — characterized by ocular pain, ocular redness and photophobia
- Insidious onset uveitis — characterized by no ocular pain and no ocular redness
- Acute uveitis — episodes of inflammation have a sudden onset and a limited duration
- Chronic uveitis — persistent relapses of inflammation occurring less than three months after cessation of treatment
- Recurrent uveitis — repeating episodes of inflammation that occur more than three months after cessation of treatment
The following diseases share some of the clinical signs and symptoms of primary iridocyclitis and the most significant differences include:
Posterior uveitis with inflammation spreading to the anterior chamber
- More likely to have significant decreased vision
- Less likely to have significant pain response
Corneal trauma
- History of ocular trauma
- Visible epithelial damage
Contact lens-induced red eye
- History of contact lens wear (often abusive)
- Corneal edema
- Corneal infiltrates
- Visible damage to corneal epithelium
Endophthalmitis
- Recent history of ocular surgery or potential ocular penetration
- Severe pain
- Severely reduced vision
- Hypopyon
- Vitritis
Acute angle closure
- Elevated IOP
- Severe pain
- Corneal edema
- Narrow / closed angle
Pharmacological Treatment
Topical Steroids
- Prednisolone acetate 1% — preferred medication; initial dosage should be aggressive, usually q1-2h for first 24-48 hours
- Durezol (difluprednate) — may also be considered at lower dosages, however, increased side effects have been reported with chronic use
Cycloplegic Agents (Moderate-to-severe uveitis)
- Cyclopentolate 0.5-2% (Cyclogyl) — can reduce ocular pain and the potential for posterior synechiae formation
- Homatropine 5% — effective in the prevention of synechiae formation
- Scopolamine — also effective in the prevention of synechiae formation
- Combination homatropine 5% and phenylepherine 10% — effective in patients where posterior synechiae already exist; act on both iris dilating muscles creating the best chance of breaking the irido-lenticular adhesions
- Phenylepherine 10% — administered to patients with cardiovascular disease
Oral Medication
- Oral prednisone — 10 mg to 30 mg daily for one week
1. Trottini M, Tolud C. The many moods of uveitis. RevOptom. 15 Nov 2013. http://www.revoptom.com/content/c/45047/. Last accessed July 11, 2014.
2. Tsang K. Iritis and Uveitis. 13 Jan 2014. http://emedicine.medscape.com/article/798323-overview#showall. Last accessed July 11, 2014.
364.01
Primary iridocyclitis
92015
Refraction
92285
External ocular photography
92286
Specular endothelial microscopy
92225
Extended ophthalmoscopy
92134
Macula OCT scan
76512
B-Scan ultrasound
76514
Corneal pachymetry
92020
Gonioscopy
92132
Anterior segment imaging
Occurence
- Estimated annual occurence is approximately 12 cases per 100,000 persons
- Maority of patients are aged 20-50
- Anterior uveitis was most common with 51.6% of patients with underlying systemic disease
- Posterior uveitis was next most common with 19.4% of patients with underlying systemic disease
Risk Factors
Underlying systemic disease
- HLA-B27
- Multiple sclerosis
- Sarcoidosis
- SLE
- Behcet’s disease
Race
- Racial predisposition to uveitis is related to the patient’s underlying systemic disease
Sex
- Uveitis does not have a gender predisposition except in cases secondary to systemic disease




 Print | Share
Print | Share